- Providers will need permission to reverse changes made in wake of covid-19, planning document says
- Permanent increase in ICU capacity planned with centralisation of specialised services
- Shared elective waiting lists across ICSs planned
The NHS in London is planning to “fundamentally shift the way we deliver health and care” in the wake of coronavirus, according to documents obtained by HSJ.
The plans from NHS England and Improvement’s London office say leaders should:
- Plan for elective waiting times to be measured at integrated care system level, rather than trust level
- Accept “a different kind of risk appetite than the one we are used to”
- Expect decisions from the centre on the location of cancer, paediatric, renal, cardiac, and neurosurgical services
- Plan for a permanent increase in critical care capacity
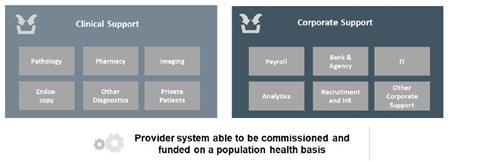
- Transform to a “provider system able to be commissioned and funded on a population health basis”
- Work towards “a radical shift away from hospital care”
- Expect “governance and regulatory landscape implications” plus “streamlined decision-making”
The document, titled Journey to a New Health and Care System, says there are three “likely” phases, with the final new system in place “from November 2021”.
The preceding two phases are “action programmes” over the next 12 to 15 months which will be about reconfiguring services to deal with “immediate covid, non-covid and elective need”, and “transition” when the move to new configurations is evaluated and “public consent” sought.
The introduction to the paper, written late last month, says: “Prior to the pandemic, the health and care system in London faced significant operational, workforce and estates pressures in acute, elective, primary care, mental health and community-based care.
“However, as we move into a period in which covid continues to circulate and remains a threat, it is clear that to be the healthiest global city, we will need to fundamentally shift the way we deliver health and care — over and above those that we planned in the London Vision and our [integrated care system] plans — if we are to control the spread of covid-19, limit its impact, address inequalities and the mismatch between need, demand and supply which existed prior to the pandemic.”
The plan involves further boosting the role of the capital’s five integrated care systems, which do not exist in law as statutory bodies.
It says “the ICS is the primary level at which the new health and care system will be designed and delivered” with the “executive and clinical leadership teams who have worked together during the pandemic response to date be[ing] the same teams to design and drive forward the new system”. It adds: “Change will be provider-led.”
In practical terms, the ICSs will have to “catalogue” changes they have already made in reacting to covid-19 with “reversal [of them] requir[ing] London approval”.
NHS England and Improvement London and ‘unhelpful distractions’
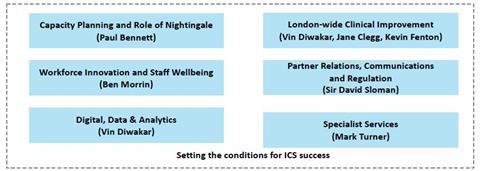
The document said the London NHSE and I regional team would “set the conditions for the ICSs to succeed” which would include “setting clinical standards” while managing the London Nightingale temporary hospital (currently not open to new admissions) and “co-ordinating London-wide pathways” in specialised services. This image shows the regional team’s workstreams:
Meeting patient need
The document says London should “maintain the total system infrastructure needed to sustain readiness for future covid demand and future pandemics”. This would mean “capacity and surge capability” in primary care, critical care, equipment, workforce, “tranportation” and supply chain.
It also moots “strict segregation of health and care infrastructure”.
System leaders should “act now” to quantify the size of the elective treatment backlog and “slow its growth as much as possible”.
The number of patients waiting more than a year for treatment is expected to have grown significantly while elective work has been cancelled.
ICS would be expected to run a single waiting list across all their providers, the plan says.
It also says there is an expectation of “disproportionate focus and resources for those with most unequal access and outcomes”.
The “risks” section of the document said it was “critical that London enables a continuation of the new culture of pace, permission and space for clinical leaders to have freedom to act during this process; accepting a different kind of risk appetite than the one we are used to”.
A senior figure in the capital told HSJ the “step change” in increased ICU capacity introduced for covid-19, and which is due to be maintained in the capital, would require capital investment. Capital would also be needed to safely segregate elective work from areas where covid-19 patients are being treated, “we rely on air flow and containment systems that often fail”, the source said.
However, remote working and remote consultations should free up office and clinical space respectively, he added.
More integration between providers
Among the other 11 “expectations” each ICS will be expected to meet are “further alignment and joining together of institutions within the ICS” and “a single, more resilient ICS-level platform for corporate support services and further consolidation and sharing of clinical support services”.
Examples listed include private patients, pharmacy and pathology.
It said the programme would be supported by “new integrated workforce and volunteer models and new incentives to drive the behaviours needed to deliver these new models of care”.
“A new approach to consent” on public engagement
The twelth “expectation” of ICSs listed in the document was a “new approach to consent through systematic deliberative public engagement e.g. citizens juries”.
NHSE and NHSI London did not clarify when asked by HSJ what role citizens juries would play and how it would sit alongside statutory obligations on public consultation, nor whether ministers had approved the plan.
The document says local authority engagement would be sought for all the priorities but especially the ones relating to shielded patients, remote consultation, reducing delayed transfers of care, same day emergency care and “community based rapid response”.
One senior figure in the capital said: “It would be great if the on-the-ground co-operation we are seeing actually persists in the longer term – but that may be optimistic.”
In a statement to HSJ, NHSE/I London medical director Vin Diwakar said: “Thanks to our staff, the swift action taken by the NHS and our partners, and the actions of Londoners in following government advice, the capital was not overwhelmed by this phase of the covid-19 pandemic.
“As the number of new patients with covid-19 falls, led by integrated care systems the NHS in London is working hard with partners to enable people to safely access health and care and to encourage Londoners to use vital services.”
Source
Document, sources
Source Date
May 2020
Exclusive: ‘Fundamental’ changes to London’s NHS in wake of covid-19

The NHS in London is planning to “fundamentally shift the way we deliver health and care” in the wake of coronavirus, according to documents obtained by HSJ.
 Currently
reading
Currently
reading
Exclusive: ‘Fundamental’ changes to London’s NHS in wake of covid-19
- 2






























19 Readers' comments