
Promotion of this article has been funded by AstraZeneca UK, who had no influence on the authors or content and reviewed for accuracy purposes only. HSJ was not editorially involved beyond minor editing for style and clarity.
Building upon the 2023 Global Initiative for Asthma (GINA) report, the recently updated British Thoracic Society (BTS)/ National Institute for Health and Care Excellence (NICE)/ Scottish Intercollegiate Guidelines Network (SIGN) guideline for asthma represents a major shift in our national recommendations for evidence-based management, recommending anti-inflammatory reliever (AIR) therapy or combined maintenance and reliever therapy (MART) over the separate preventer and reliever approaches that had previously been the mainstay of asthma care.3,4
Moving away from reliance on short-acting beta agonist (SABA) reliever inhalers towards approaches using AIR or MART is expected to reduce asthma exacerbations, prevent hospital admissions, and decrease premature mortality.3-6 However, modifying long-established patterns of behaviour and management can be challenging, requiring education and support for clinicians and for people with asthma, amidst the multiple competing pressures within general practice.
To improve asthma-related outcomes, a multifaceted initiative to transform asthma care was launched in Bedfordshire, Luton and Milton Keynes (BLMK) Integrated Care Board following publication of the GINA report in 2023. This was designed to enhance competency and confidence in offering evidence-based management in line with the report’s recommendations, to provide practical approaches to identify, prioritise and address unmet need, and to resource and recognise consistent best practice.
Enhancing competency and confidence
The ICB programme team and clinical lead designed a suite of resources for clinicians and delivered education through various channels. This included updating the BLMK asthma guidelines, specific sessions on asthma management, as well as protected learning time events, along with the dissemination of a one-page summary in the GP bulletin and through direct communications to practices. Each primary care network identified a respiratory champion, and a community of practice was created, facilitating the sharing of learning and approaches to common challenges.
Practical approaches for proactive care
Clinical searches were developed using objective criteria to identify potential SABA overuse and likely underuse of inhaled corticosteroids (ICS). The highest-priority cohort included people prescribed six or more SABA inhalers in the previous 12 months without any ICS; practices were supported to run these reports to proactively identify people with unmet need. In parallel, alerts were built to highlight improvement opportunities when records were accessed and software on clinical systems was configured to encourage optimal evidence-based prescribing.
Resourcing and recognising best practice
Pump-priming funding was made available to early adopter PCNs to resource time for training and clinical reviews. The following year, this was expanded to all practices through the prescribing incentive scheme, with practices encouraged to clinically review and offer appropriate therapy to people with asthma who have been prescribed six or more SABA inhalers in the previous 12 months. Concurrently, additional incentivisation was introduced through the BLMK Primary Care Framework, with remuneration directly linked to performance on objective measures of SABA overuse. These schemes worked synergistically to support and reward the adoption of best-practice pathways, while raising awareness of the dangers of SABA overreliance. In the absence of a systematic national audit providing practice-level data, the ICB has continued to update practices with quarterly data on performance and benchmarking.
How well did the programmes work?
In the 2024/25 financial year, more than 4,500 people with asthma were recorded as being offered AIR or MART therapy. More than two-thirds of those who were clinically suitable took up the offer and had a change in treatment. There was a marked reduction in SABA prescribing with a 30 per cent drop in the number of people with asthma prescribed six or more SABA inhalers in the previous 12 months (from ~8,500 to fewer than 6,000). This has led to BLMK becoming the fifth best-performing ICB nationally on this measure.7

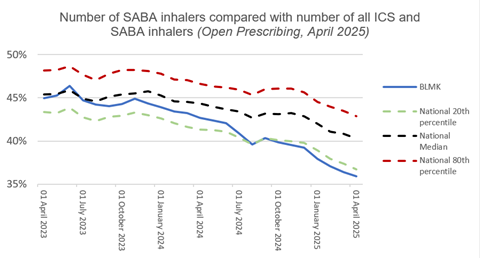
The improvement compares favourably with that seen overall in England; from April 2023 to March 2025, BLMK ICB moved from alignment with the national median for SABA inhaler prescribing relative to all ICS and SABA inhalers to being positioned within the best-performing quintile.8
As well as the clinical benefits, this has reduced the environmental impact of asthma care in BLMK; with a 25 per cent drop in salbutamol inhalers issued quarterly over this timeframe (~93,000 to ~70,000), an estimated carbon footprint of nearly 1.5 million kg CO2 e has been averted over two years — the equivalent of almost 7 million petrol car miles.9,10
What’s next?
Having fulfilled its purpose of raising awareness of the new BLMK asthma guideline and enhancing competence and confidence with AIR and MART approaches, financial support through the prescribing incentive scheme has now been retired. However, the BLMK Primary Care Framework incentive for avoidance of SABA overuse has been maintained into 2025/26, with each iteration of data continuing to reveal ongoing improvement. Our next steps to understand the full impact of these changes in practice will include analysing hospital admissions and additional outcomes.
This initiative in BLMK ICB demonstrates how a multifaceted approach to improving asthma management has resulted in marked clinical and environmental benefits. We would encourage systems to explore similar approaches, including support to enhance competence and confidence in providing evidence-based care, provision of practical tools for population health management and quality improvement, and appropriate resourcing and recognition of best practice.
Veeva ID: GB-72021
Date of preparation: November 2025
References
1 Asthma + Lung UK. What is asthma? (2024).
2 Asthma + Lung UK. Estimating the economic burden of respiratory illness in the UK. (2017).
3 Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention. (2023).
4 NICE. Asthma: diagnosis, monitoring and chronic asthma management (BTS, NICE, SIGN). NG245. (2024).
5 MHRA. Drug Safety Update. Volume 18, Issue 9: April 2025
6 BLMK Respiratory Group. Asthma Guidelines for Adults (2024).
7 ePACT2 Respiratory Dashboard (accessed 10th September 2025).
8 OpenPrescribing. Short acting beta agonist inhalers in BLMK ICB. (accessed 10th September 2025). https://openprescribing.net/sicbl/M1J4Y/measures/?tags=respiratory
9 OpenPrescribing. Environmental impact of inhalers in BLMK ICB. (accessed 10th September 2025). https://openprescribing.net/measure/carbon_salbutamol/sicbl/M1J4Y/
10 OpenCO2net. CO2 converter. (accessed 10th September 2025). https://www.openco2.net/en/co2-converter

































