This article was initiated, written and funded by Boehringer Ingelheim

Interstitial lung disease (ILD) describes more than 200 rare and complex lung conditions. The most common fibrotic ILD is idiopathic pulmonary fibrosis (IPF), which has a median untreated life expectancy of just three to five years from diagnosis.[1] This makes timely and accurate identification, as well as rapid referral for diagnosis and specialist care, absolutely critical.
Access to specialist services is uneven across the UK, with many people facing long waiting times and long journeys for diagnosis and treatment.[2],[3] For people living with ILD, whose disease progression can be rapid, delays or interruptions to their care can be life-altering. The symptoms of chronic breathlessness, an ongoing cough and fatigue can be debilitating and make travel to a specialist centre for diagnosis and ongoing care even more difficult and distressing.

The NHS 10-Year Health Plan prioritises care closer to home, aiming to delegate services and empower local systems.[4] This vision is relevant for those living with ILD, whose needs are complex but manageable with the right infrastructure. The plan’s emphasis on digitally enabled care and integrated and community-based services offers impetus for driving timely, holistic and equitable ILD care improvements.
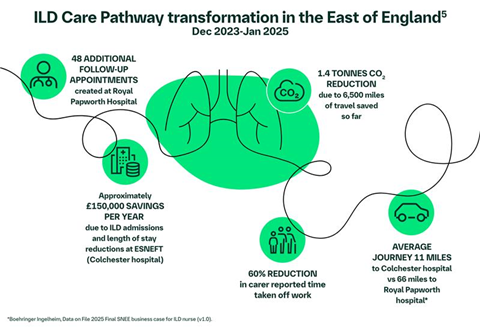
A compelling example of this vision in action is the collaborative partnership between Boehringer Ingelheim, Royal Papworth Hospital Foundation Trust, and East Suffolk and North Essex FT (Colchester Hospital). The project redesigned the ILD care pathway to deliver specialist services locally, streamlining diagnostics, reducing repeat testing and minimising travel. Patients receive timely, expert care without the burden of navigating multiple appointments across distant locations. This model enhances efficiency, reduces system costs, and leads to high patient satisfaction.[5] This approach aligns closely with the OneVoice ILD Care Pathway, a nationally endorsed framework developed by clinicians, patients and patient charity Action for Pulmonary Fibrosis. One of the key recommendations is the creation of new “Tier 2” specialist centres to alleviate capacity pressures while providing care closer to home.[3]
Updates to the ILD service specification and creation of new local commissioning standards provide an opportunity to modernise ILD services and codify best practices such as access to a specialist nurse, virtual multidisciplinary teams (MDTs), and integrated care models. Evidence suggests that ILD prevalence has been increasing across the UK,[6] so these standards must be future-proofed as well as reflect the aspirations of ILD leaders, clinicians, patients and patient organisations alike.
ILD remains far less prevalent than other respiratory conditions like chronic obstructive pulmonary disease or asthma. To prevent ILD from becoming a forgotten disease, it is important to embed it within broader respiratory and public health strategies, such as:
- Raising awareness to improve early recognition, including among primary care practitioners and rheumatologists (due to the increased risk for patients who have rheumatoid arthritis and other systemic autoimmune diseases)[7]
- Integrating ILD services into population-based respiratory or breathlessness pathways, to be considered alongside diseases like COPD and heart failure
- Expanding access to diagnostics, such as high-resolution CT scans and lung function testing in community settings
- Investing in virtual multidisciplinary teams and clinics to support local clinicians with specialist ILD input
The success of the Royal Papworth-Colchester model demonstrates that innovation is possible, even within existing constraints. To replicate this success nationally, we need ongoing policy alignment and leadership, strategic investment and cross-sector collaboration.
Find out more about Boehringer Ingelheim’s Human Health Collaborations here www.boehringer-ingelheim.com/uk/partnering/human-health-partnering
NP-GB-106184
January 2026
References
[1] Wijsenbeek M et al. Interstitial Lung Diseases. Lancet. 2022;400:10354,769-786.
[2] Fahim A et al. Idiopathic pulmonary fibrosis in the UK: findings from the British Thoracic Society UK Idiopathic Pulmonary Fibrosis Registry. BMJ Open Respiratory Research. 2025;12:e002773.
[3] OneVoice ILD. Interstitial Lung Disease Care Pathway. Available at: https://www.actionpf.org/get-involved/transforming-ild-services.
[4] NHS. Fit For The Future: 10 Year Health Plan for England. July 2025.
[5] Fiddler, C et al. 2025. A retrospective evaluation of a novel specialist shared care ILD pathway. Poster ID 3012, ERS Congress.
[6] Whittaker, H et al. Incidence and prevalence of asthma, chronic obstructive pulmonary disease and interstitial lung disease between 2004 and 2023. Thorax, 2025;80:466-477.
[7] Dong YX et al. Advancing understanding of autoimmune disease-related interstitial lung disease (AD-ILD): A global perspective on research focus and future directions. Autoimmunity Reviews. 2025;24(1): 103697.


























