The establishment of 42 integrated care systems ushers in an unprecedented opportunity to deliver wide ranging improvements in population health and care as well as wider system performance. If that potential is to be realised, digital and analytics will need to play a central role.
How can ICS leaders grasp this opportunity?
Sponsored by
The potential value at stake is significant, and so is the need
The potential of digital, data and technology to enable enormous improvements in health and healthcare is now widely accepted.
Globally, leading health systems are delivering leaps forward in data-driven population health management, digitally-enabled care pathways, real-time demand and capacity planning and wide-ranging advances in research and innovation. Improved use of digital and data lies at the heart of every leading health system’s attempts to improve outcomes, experience, access and overall sustainability.
While health has often been accused of lagging behind other industries in digitally-enabled transformation, the past two years has seen a dramatic acceleration. In the NHS, clinicians in hospitals and care homes are now able to make better, quicker and more informed decisions about a patient’s treatment as a result of improved access to GP records; and this has been accompanied by well-documented advances in the adoption of broader digital health and care services.
At the same time, following the pandemic, the pressures facing the NHS and social care are more acute than they have ever been. Understanding and taking advantage of the opportunities for data, digital and technology to unlock improved outcomes, experience and productivity could barely be more urgent.
What needs to be different?
While the NHS on average spends £4bn per year on IT[1], this is often highly diffused across subscale delivery of disconnected local solutions that increase technical debt and are not designed to scale, and as a result, are not set up to realise the full value for patients and staff.
ICSs have been created to enable collaboration across previously subscale and siloed organisations, funding flows and services. They also provide the key to unlocking digital, data and technology-enabled transformation.
A new approach
Driving an ICS-wide digital, data and tech transformation, and unlocking the associated economies and scale and skill, will require new capabilities and a fundamentally different approach and operating model at both a national and system level.
Such changes often require multiyear efforts to evolve current governance, funding, skillsets, mindsets, and capabilities – which may seem daunting. How can ICS’s get started in the meantime? Through analysis of leading international health systems and interviews with leaders on the journey to establish as ICSs, we’ve identified five “first step” success factors:
1. Anchor the digital, data, and tech strategy in overall target outcomes for the ICS
Nationally, the integration of NHSX and NHS Digital within NHS England seeks to remove the silos between strategy and delivery as well as the unhelpful distinction between overall system strategy and digital strategy. At ICS-level, this is just as important. The digital, data and tech strategy and accompanying roadmap need to be fully integrated and aligned with the broader ICS strategy and the outcomes it is seeking to deliver.
Given budgetary pressures, the appropriate balance will need to be found between initiatives ensuring minimum tech, data and security foundations, and strategic investment to deliver ambitious ICS health and care outcomes.
2. Streamline governance for system-wide digital, data and tech decision-making
ICS-wide prioritisation and investment decisions should be enabled through a recrafted governance and funding approach. Decision rights will need to be defined and supported by collective agreement from technology, clinical, operational and finance leads who represent the breadth of system perspectives. Agreement on which initiatives will be prioritised, funded and implemented at the system level, versus by individual organisations, and therefore how and when to pool budgets to support ICS-wide priorities, will be critical.
3. Appoint an ICS-level executive leader for digital, data and technology
System-wide transformation benefits from a leader with a system-wide mandate for bold and holistic change across digital, data and technology. This means bringing the singular focus of a deeply expert leader who has the experience, delivery accountability and convening power to mobilise other ICS leaders around a clear strategy and priority initiatives. However, the potential of digital, data and technology cannot be realised by solely one individual, but is a collective responsibility of all ICS executives who are equipped to be digitally literate with the appropriate training and support.
4. Establish an ICS Digital, Data and Tech Transformation Office
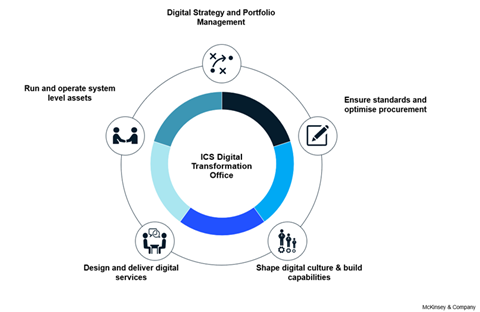
Delivering the ICS portfolio of digital, data and tech transformation initiatives can best be enabled through an execution team that brings together and upskills often fragmented and underequipped digital, analytics and technical teams from across the system. This small ICS-level team is crucial to facilitating collaborative, system-level transformation and delivery (see exhibit), with provider and place-based leaders supported by the necessary expert capabilities and specialist skills (eg, design, modern technical architecture, product management).
5. Break down the silos between disciplines and organisations
Technical changes are the tip of the iceberg and the easiest part of digital-enabled transformations. The hardest part – and the unlock to value capture – are the people and process changes entailed in the adoption of new technology-enabled ways of working or new models of care. For example, while replacing ageing LIMS systems is a significant technology upgrade, the real value comes from the shift to an ICS-wide laboratory network. Such change is possible when ICS decision-making and delivery evolves from siloed organisations and functions to a multidisciplinary operating model of clinical, operational, and technology teams jointly deployed from different organisations against ICS priorities.
Five early tests
While the principles of a new system-wide approach and operating model for digital, data and technology may be simple, implementation is anything but.
The early indication of whether ICSs are moving in the right direction will be come through five tests:
- Is there an agreed list of prioritised, ICS-wide digital, data and technology initiatives that clearly link to overall system priorities and target outcomes?
- What percentage digital, data and tech funding has been pooled to support ICS priorities?
- Who is the executive owner of the digital, data and tech agenda with an ICS-wide mandate?
- Has a digital, data and tech transformation office been set up and resourced to drive execution?
- How many projects are delivered by multidisciplinary teams, from across different organisations, working together towards delivery of ICS priority initiatives and outcomes?
As ICSs embark on this journey, the challenges ahead are significant, but the opportunities to improve outcomes are greater.
References
[1] Laing & Buisson, Digital Health UK report, 2nd edition. Average spend is £4bn for England and £5bn across the United Kingdom, with high levels of variability across individual trusts.


























