As rollout of the NHS Federated Data Platform (FDP) nears completion, it offers a transformative opportunity to improve performance and patient outcomes. Fulfilling this potential will need a coordinated focus on value by the NHS, and spirited buy-in from across the healthcare ecosystem. In this article, we outline six ideas to unlock the FDP’s potential in the near term.

Sponsored and written by
“We need something like this in our country!” This is a typical comment we hear from our international publicly-funded health system clients when they understand the NHS Federated Data Platform programme and the potential impact it promises. As a result, we have been closely tracking the FDP’s progress, interviewing NHS leaders engaging with the technology, and thinking about how to maximise the benefit from the investment the NHS has made. Our full perspective, summarised in the article below, can be found on our website.
Rollout of the FDP across the NHS estate is putting secure, integrated and standardised data into the hands of clinical and operational decision-makers in a way that could revolutionise NHS working practices. It has the reach and capability to solve the interoperability challenge; become the primary vehicle for a unified patient record; drive at-scale delivery of applied AI solutions; and underpin the cross-organisation coordination of care necessary for the government’s shifts towards community-based care and prevention over treatment.
In so doing, it provides a generational opportunity to transform patient experience and outcomes. In a future unlocked by the FDP:
- A diabetes patient could receive a notification via the NHS App to take their daily exercise, prompted by remote monitoring of their physical activity against a health promotion and longevity plan generated by AI, based on their lifetime care record and refined by them and their GP
- A clinician could benefit from automated decision support, driven by the full care record of the patient in front of them and the full history of patient outcomes in the NHS, that guides the clinician to the optimal treatment, offers the next best action or referral they could take, and orders tests and prescriptions without duplication
- A care planning AI model could track real-time movement of patient cohorts along care pathways between acute and community settings, identify bottlenecks in patient flow and redirect capacity accordingly
- An academic researcher could connect to national-scale anonymised health data and use this in their research, accelerating the development of life-saving therapies by analysing treatment outcomes and uncovering genetic markers of disease
“Having joined-up decision-making across care settings would be a truly brilliant outcome from the integrated system data that FDP is facilitating,” according to Daniel Elkeles, incoming CEO of NHS Providers and outgoing CEO of London Ambulance Service. “It is an opportunity that the NHS must not miss”.
At the same time, McKinsey’s research into the potential value that can be unlocked from digital and data use-cases deployed at scale suggests there is an opportunity equivalent to £15-25bn per year in the UK¹, while decommissioning “tech debt” systems rendered superfluous by the FDP could alone pay for the rollout. “We should start to see cash out in local systems as we can start to reduce our reliance on local infrastructure,” says Will Monaghan, chief digital information officer for two Midlands trusts.
However, we know from our global public sector and tech research and from the NHS’s own track record of large-scale technology programmes that the deployment of technology alone is never enough to unlock value. We see six ideas to ensure that the investment in a core technology platform can improve patient outcomes:
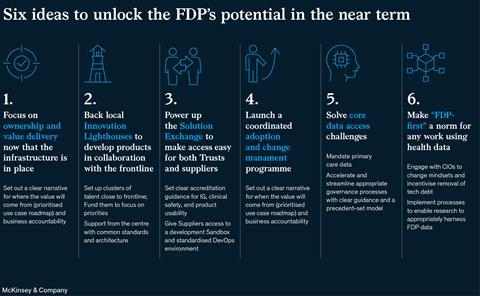
- Focus on ownership and value delivery from the infrastructure by pairing tech leadership with “active customers” of FDP products accountable for impact, and laying out the sequence of concrete use cases and the outcome targets they seek to deliver
- Establish and back Innovation Lighthouses where technical talent and frontline users work side-by-side to create robust, scalable and high-impact solutions on the FDP that fit seamlessly into operational workflows
- Power up the FDP Solution Exchange by making it easy for trusts to find and deploy accredited products, and giving suppliers access to a development sandbox, standardised DevOps environment and clear development guidance
- Launch a coordinated adoption and change management programme to show trusts how they can benefit, ensure staff are trained, incentivise product usage, coordinate integrated product deployment and monitor impact
- Solve core data access challenges by including GP- and even local authority-held data in FDP, and streamlining appropriate governance processes with clear guidance and a precedent-setting model
- Make “FDP-first” a norm for any work using health data, including by incentivising removal of tech debt and harnessing the full power of the FDP for use in research (with the appropriate pseudonymisation, research governance and permissions)
Fulfilling the transformative potential of the FDP will need a coordinated focus on value and outcomes across the NHS: from executive leadership and operational delivery to frontline usage and patient support. It will also need spirited buy-in from across the healthcare ecosystem of policy-makers, NHS operators and clinicians, suppliers, life sciences organisations, academia and beyond – all of whom stand to gain from its success. If the NHS can put these pieces in place, it can unleash the full potential of the FDP vision, unlock an opportunity for sector-leading digital transformation, improve health system performance, and significantly advance patient care and outcomes.
Note:
¹ McKinsey’s Digital Value Assessment evaluates how much health systems stand to gain by implementing next-generation clinical systems, optimising patient flow, capacity and supply chain distribution across healthcare systems, enabling patients’ management of their own care, and supporting population health for better health promotion and disease prevention. It builds on an extensive evaluation of the potential impact of these use-cases from academic literature, and assesses what proportion of the total opportunity still remains to be captured within a country or health system.

























