The “friends and family test” might not be universally popular in the NHS, but it can help bridge the listening gap between patients and organisations, write Jonathan Nicholls and Ben Page

It’s fair to say that the “friends and family test” has not been received with universal rapture by the NHS.
The objections? Patients don’t like the question; the different patient case mix across the country and different sites mean comparisons are not valid; the different data collection methods introduce bias; the test doesn’t provide the detail to improve services; and so on.
But are these criticisms really the best thing to focus on? Ministers have decided the friends and family test is here to stay − for now at least − so perhaps a more useful question is: whatever its limitations, how can providers use it to improve services for patients?
‘A common perception appears to the NHS is not great at listening to – and, by implication, dealing with – concerns’
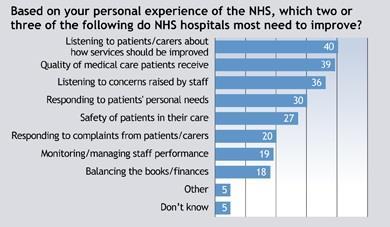
A new Ipsos MORI survey, published exclusively on hsj.co.uk today, suggests there’s a job to be done, at least from a public perceptions point of view. We asked people answering the survey to prioritise areas for NHS improvement, drawing on, among other things, some of the issues identified in the Francis report.
What comes across starkly is a public perception of a “listening deficit” in the NHS. Despite overall satisfaction levels holding up well, 40 per cent still believe the NHS should be better at listening to patients, and 36 per cent say it should be better at listening to staff.
A common perception appears to be that the NHS is not great at listening to − and, by implication, dealing with − concerns. Over the past two decades we have consistently found this − often people are inhibited about complaining because of the NHS’s revered national status.
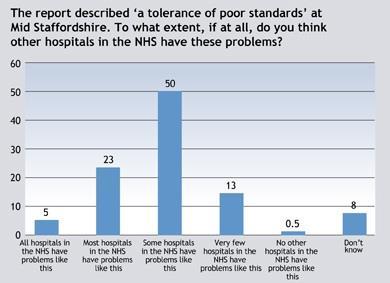
This listening gap resonates with the Francis report, something Robert Francis refers to as a “tolerance of poor standards”. Perhaps more worrying for the NHS is the public perception of how widespread this is. Nearly 30 per cent of the public think this tolerance of poor standards happens in most or all NHS hospitals, with one in 20 thinking the problem is endemic.
Looking beyond the question
So how can the “friends and family test” help? Well, the critics are right: by itself, the test question can’t do much to change this. But the test guidance tries to encourage trusts to look beyond asking just the single question. As a minimum, they should also ask patients why they gave their rating − a rich source of insight into how patients view their services.
More importantly, the guidance also expects trusts to ask locally determined follow-up questions. It’s these questions that can be really key in closing the listening gap. But to do this providers need an effective strategy for patient-led service improvement.
‘The test can be invaluable for delivering patient-led service improvement’
What this means in practice is not defaulting to standard national questions on issues such as dignity and respect, communication and so on. These are important and have their place, but there’s an argument that focusing exclusively on standard questions de-skills managers from thinking about “what really matters to my patients, and how do my patients want those issues addressed?”
This is well established in the commercial sector through processes like customer journey mapping: work closely with customers, systematically identify the service touchpoints that matter to them, design the service to deliver good touchpoint experiences, then track customer views to make sure the touchpoints are delivered well and the customers are happy.
Here, despite the criticisms, the test can be invaluable for delivering patient-led service improvement. While there are problems comparing test scores across services, you can track scores in a given setting over time. So by using the follow-up questions to ask about the critical patient touchpoints, you can track how well you are delivering those touchpoints − and whether this is moving your overall test scores in the right direction.
By itself, this doesn’t mean things will improve. Organisational factors such as unclear leadership, disengaged staff or poor staff empowerment can get in the way. If your score isn’t improving, this is where you need to look. The self-assessment toolkit we developed with the NHS Institute for their “patient feedback challenge” is a free resource for the NHS and a useful starting point.
Complex challenge
Even so, this remains a complex challenge, and Ipsos MORI and King’s College London will be working with NHS patient experience leads over the summer to examine this more closely: what do providers need to do to get beyond the metrics to drive substantive improvements in patient experience? We will share our findings later this year.
In the meantime, the public perception of a listening deficit should be a concern to the NHS. If it’s implemented well the “friends and family test”, with the right follow up questions, provides an opportunity to start closing that gap.
Jonathan Nicholls is head of health research and Ben Page is chief executive of Ipsos MORI, a company which offers trusts services to collect patient feedback























10 Readers' comments