South London and Maudsley Foundation Trust has successfully reduced the number of patients admitted to private psychiatric units. Kamran Ahmed and colleagues explain how the private overspill review team turned it around

During the past few years there has been an exponential increase in the number of patients being admitted to private psychiatric units from NHS mental health trusts in the UK due to their inability to meet the demand for admissions within their own bed capacity.
‘The resulting patient “overspill” into psychiatric beds in the private sector is costing the NHS millions’
There are several causes for this, including:
- population growth;
- the restructuring of community mental health services and;
- a reduction in acute psychiatric beds.
More than 1,700 mental health beds were closed between April 2011 and August 2013 - an overall reduction of 9 per cent - primarily as a result of budget cuts to the majority of England’s 47 mental health trusts.
- Use the Change Challenge interactive tool
- Sign up to receive the weekly innovation and efficiency newsletter
Increased referrals and occupancy
Average occupancy levels in acute adult and psychiatric beds continue to run at 100 per cent according to freedom of information figures from 28 trusts. Half of these providers had levels of more than 100 per cent and allhad occupancy rates above the 85 per cent recommended by the Royal College of Psychiatrists.
Referrals to crisis and community mental health teams are reported to have risen by 16 per cent in the past two years. This increasing demand for mental health services is thought to be due to a reduction in resources, the effect of the economic recession and welfare reform.
‘The financial implications of the figures have put considerable pressure on the trust’
The resulting patient “overspill” into psychiatric beds in the private sector is costing the NHS millions. In 2013 Manchester Mental Health and Social Care Trust reportedly spent £1.75m in four months sending patients to out of area private hospitals due to a shortage of NHS beds.
At South London and Maudsley Foundation Trust 542 patients were admitted to private beds in 2013. The average length of stay in private care was 21.3 days for female patients and 27.8 days for male patients.
With an average cost of around £495 per day, the financial implications of these figures have put considerable pressure on the trust, and patients receive poorer quality care due to isolation from their support networks.
The dream team
In response to the increasing number of patients in private overspill, the trust set up a multidisciplinary workstream which put a number of different operational and capacity management initiatives into place. Home treatment capacity was increased and two 13 bed internal overspill wards were opened in December 2013.
‘The overspill review team helps reduce length of stay by advising external providers’
At the same time, the trust worked with commissioners to approve plans to launch a significant investment in community services to deal with systemic issues, focus on high caseloads and improve therapeutic interventions.
Also, a private overspill review team was set up on a short term basis in January last year to provide assertive in-reach for patients admitted to private units.
The team’s function was to improve the quality of care provided to the trust’s patients in the independent sector and to reduce their length of stay by advising external providers on treatment, improving communication between trust and external providers, and to help facilitate timely discharge.
The private overspill review team consists of the following members:
- Clinical service lead: Oversees all activities and supports the team; organises the repatriation to trust beds of specific patients as identified by clinical team members; and feeds back to the trust bed management meeting regarding private overspill and escalates delayed discharges there.
- Consultant psychiatrist: Conducts weekly face to face reviews or telephone discussions with private ward consultants for all patients in the private sector with a view to advising on treatment, care planning and discharge options; provides clinical leadership to the team and feeds back clinical updates, discharge plans and estimated discharge dates to rest of review team; and has an overview of the quality of care being provided to patients in the private sector and feeds back at the trust bed management meeting if any concerns are identified.
- Home treatment team practitioner: Carries out all assessments and clinical reviews for patients identified as suitable by the consultant and facilitates their discharge to home treatment teams; and refers patients to discharge coordinator to facilitate discharge.
- Discharge coordinator: Provides discharge/care coordination for those patients admitted to the private sector whose discharge is complex as identified by consultant/home treatment team practitioner; and liaises with community teams and complex care services as appropriate to ensure their involvement with patients and assistance with discharge.
- Head of service development: Provides operational oversight of the systems within the private overspill team.
- Medical administrator: Provides administrative support to the review team; and daily updates to private overspill patient list to monitor which patients have been admitted to private overspill and which ones have been discharged or transferred.
Developing an operational policy
During the time that the review team was functional, a service development project was initiated to improve team processes and in doing so, to improve the quality of care given to patients admitted to the private sector and reduce their length of stay.
A stakeholder analysis was carried out and the project team members conducted interviews with members of team, trust executives, a patient and their relative, private unit clinical staff and members of the trust bed management meeting. A process map was also drawn up to identify potential areas for improvement in how the review team worked.
The following recommendations were made and implemented for the team:
- The team would check for new admissions to private overspill beds on a daily basis and discuss with bed management if necessary;
- A daily morning team meeting to discuss all patients in private overspill would be conducted with the aim of reviewing all patients in overspill, including diagnosis, treatment plans, progress and discharge date including potential barriers to discharge;
- The team would make contact with the private hospital where a patient is admitted and the patient’s care coordinator or community mental health team within 24 (for weekday admissions) or 72 hours (for weekend admissions) to share information and plan treatment and discharge;
- The team would ensure that each patient admitted to a private unit has hard copies of the following where available: admission clerking, section papers, last 50 entries from the electronic notes system, risk assessment, previous discharge summary, care plan, contact details of care coordinator;
- For patients transferred from a trust to private inpatient bed, or vice versa, the following additional information should also accompany them – vital signs chart, patient property list, prescription chart, verbal nursing handover, verbal medical handover;
- The team would conduct face to face reviews of all patients admitted to private overspill within 72 hours with a view to care and discharge planning.
- Ongoing weekly reviews of patients admitted to private beds and telephone discussions with clinical staff.
At the same time, other wider changes were made at the trust including:
- the creation of additional acute inpatient bed capacity (26 beds);
- to have the same operational policy for all home treatment teams regarding patients in the private sector and work flexibly in taking them on;
- community mental health teams having a separate policy for patients in the private sector outlining the requirements for making contact and visiting them on the ward and providing follow up on discharge;
- bed management informing the review team (medical administrator), the relevant community team leader, care coordinators and relatives at the point of patient transfer/admission to private sector and ensuring that the admitting clinician is aware of the checklist of information to be sent;
- the admitting clinician would provide the following documents with every admission to the private sector where available: admission clerking, section papers, last 50 entries on electronic medical record system, the risk assessment, previous discharge summary, the care plan and contact details of the care coordinator;
- designing a screensaver regarding private overspill to be featured on all trust computers to encourage all professionals to work together to tackle the issue; and
- implementing a “senior medical manager on call” rota in April last year so that all admissions to trust and private beds between 9am and 12am would be discussed with a senior experienced clinician who could explore alternatives to admission.
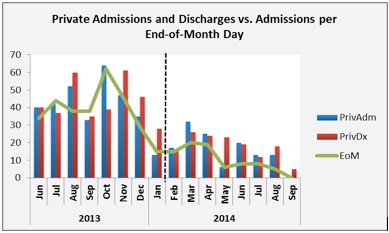
As shown in the graph above, through the review team’s work, the other operational changes and increased capacity at the trust, the number of patients in private beds reduced from 65 in October 2013 to 0 by September 2014 (EoM represents the number of patients in overspill at the end of each calendar month).
The review team has been deemed an effective contributor to a reduction of patients in private overspill beds. It is an approach that other trusts can use to deal with patient overspill.
Dr Kamran Ahmed is a consultant psychiatrist; Dr Nkechi Iwegbu is locum consultant psychiatrist; Muhammad Ishrat Husain is an ST6 higher trainee; Dr Wendy A. Addae is an information analyst and Dr Martin Baggaley is medical director, all at South London and Maudsley Foundation Trust



























1 Readers' comment