![]()
This is paid-for content from our commercial partners. Find out more
The Coronavirus (COVID-19) pandemic has highlighted a clear need to re-evaluate existing referral pathways within renal services, in order to prioritise a more pro-active, planned and person-centred approach to shared decision-making – and crucially to avoid costly unplanned suboptimal care. The management of kidney failure is one such pathway.
Sponsored by
NHS renal services manage individuals with kidney failure, which may occur as a result of chronic kidney disease (CKD) or acute kidney injury (AKI). Around 3 million people in the UK today have CKD – with uncontrolled diabetes and high blood pressure the biggest causes. Currently 63,000 of these people are being treated for kidney failure (stage 5 CKD) and each day 20 people will need to start Renal Replacement Therapy.
In England around 6,714 people start renal replacement therapy (RRT) each year; 8% will have a pre-emptive transplant, 20% will start on peritoneal dialysis (PD) and 71% will start on haemodialysis (HD), which is given in hospital at a satellite centre or at home.1 There was an 11% reduction in dialysis patients and an 8.5% drop in stage 5 CKD patients attending hospital over the March to June 2020 period in comparison to the prior two years.2
For patients who are stage 5 CKD, the ideal situation would be the option of a kidney transplant, this is not always suitable nor available for everyone either because of a lack of available donors, medical complications or patient choice. There is evidence of huge variation in the recognition and care management of kidney failure across the country and the need for focused improvements cannot be overestimated.
Working in partnership with Baxter Healthcare Limited, Wilmington Healthcare Consulting developed a fictional – but robust Costed Integrated Patient Scenario (CIPS) in order to fully evaluate the existing range of dialysis options for people with progressive CKD not eligible for transplant. This enabled clear identification of the key health and social care components that would comprise an optimal best practice pathway through a full comparison of planned proactive versus unplanned reactive RRT. The following approach was undertaken:
(1) MDT stakeholder review covering all aspects of the pathway to be evaluated, from presentation of the individual with CKD, through specialist intervention to managed care in the community
(2) Construction of a strawman (Sid) to guide the process; the core background narrative for a realistic, but fictional renal patient including some initial base level pathway assumptions
(3) Utilisation of a three round iterative Delphi3 process with the expert MDT panel to construct the patient scenario and development into a case study text
(4) Economic analysis of all health, social care, service user costs between the ‘new’ approach and the existing standard of care is then applied in order to highlight individual choice elements and the potential service improvements that could be implemented.
Management of kidney failure, like many other conditions requires collaborative working across all areas of the health economy so that there can be a smooth, fast and efficient flow between health professionals to recognise kidney deterioration and ensure a solution is not missed and that the individual with CKD is provided with the right support and information to make the best choice. The evidence derived from this CIPS evaluation reinforces this and indicates that pre-emptive early diagnosis and prompt treatment of CKD in primary care leads to significant reduction both in overall cost and a shift from expensive and avoidable secondary care management.
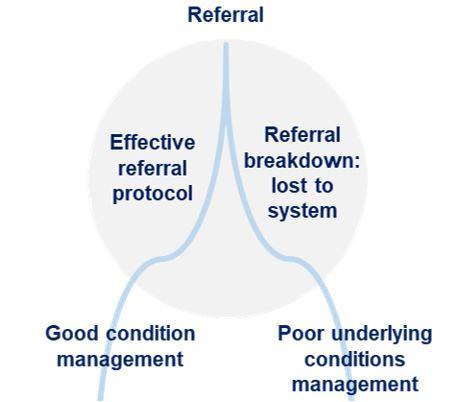
Figure 1: The critical window in the CKD care pathway
Early intervention in primary care during the ‘critical window’ within Sid’s optimal scenario is the opportunity to improve his health outcome, his quality of life and the overall cost of his care. It enables those involved in delivering care to identify his progressive CKD early and ensure onward referral into specialist renal services for proactive assessment and continued MDT management of his CKD. Additionally, the optimal scenario highlights the collaborative use of Digital Health records shared between clinical teams, as well as referral guidelines to further optimise local GP monitoring and enhance patient involvement and enablement.
Furthermore, with the advent of Integrated Care Systems from April 2021, there is not only a need to understand the overall cost of the total CKD journey -from an integrated care service with integrated budgets – but also the impact of future integration of renal home therapies into regional or network decision-making that focuses on proactive budgeting, resource and capacity planning. Table 1 clearly highlights a summary of the total financial costs of not proactively managing CKD – a difference of over £150,000 per patient for the total CKD journey over the years documented in this CIPS.
Table 1: Full financial summary of NHS costs
| Cost driver activities | Suboptimal | Optimal |
|---|---|---|
|
Acute |
£220,185 |
£64,736 |
|
Ambulance service |
£444 |
£0 |
|
Community teams |
£0 |
£1,250 |
|
Primary care |
£4,026 |
£3,328 |
|
Total |
£224,655 |
£69,314 |
N.B. Financial costs are indicative and calculated on a cost per patient basis
This serves to highlight that proactively managing Sid’s progression to renal failure from earlier identification and management within primary care, improved the overall experience of the acute admission, his after care and the overarching clinical pathway costs. This CIPS evaluation is therefore intended to help renal commissioners and providers understand the implications in terms of quality of life and the financial costs of shifting the care pathway of people living with CKD from costly unplanned reactive care to a more proactive, planned and person-centred approach – particularly as regional decisions to transform care pathways begin to acquire a population view of costs and improvement over the medium-term.
Identifying all elements of Sid’s journey could enable greater investment earlier in the patient journey and ensure personal choice of modality for RRT therapy is always considered. This is even more pertinent in the post coronavirus pandemic environment, which has had a profound impact on the NHS and placed unprecedented demand on renal services and dialysis delivery. The crisis has emphasised a clear need to evaluate existing referral pathways and the rapid introduction of virtual care models in parallel to support increased home dialysis provision for new incident patients.4
References:
1UK Renal Registry 22nd Annual Report. Data to 31/12/2018 Chapter 1 Adults starting RRT for end-stage kidney disease (ESKD) in the UK in 2017 https://www.renalreg.org/wp-content/uploads/2020/07/22nd_UKRR_ANNUAL_REPORT_Ch1.pdf
2Covid Tracker Tool; Wilmington Healthcare, accessed September 2020
3The Delphi Method. Wikipedia (2020) https://en.wikipedia.org/wiki/Delphi_method
4NICE (2020), Covid-19 rapid guideline: dialysis service recovery https://www.nice.org.uk/guidance/ng160



























