There are five things we can do to keep us mentally well that we can also use to manage and monitor our health outside the NHS. They can do more for us than the health service can, argues Philip Hammond
“I’ve been fighting Crohn’s disease for control of the body we both inhabit for as long as I can remember. I was finally diagnosed in the spring of 1983, when I was 19, after seeing 17 different GPs in my desperate attempt to prove I wasn’t a neurotic hypochondriac causing my own gut spasms, diarrhoea and blood loss.
“The relief of being told I had a ‘real’ disease cannot be overestimated. The fact that I was told I must have had it for 15 years for it to be in the state it was, was air punchingly satisfying.
“From then on, my care from the NHS has been fantastic. But I had to work to make that happen as well. You can’t just sit back and hope the NHS will look after you; you have to stay on top of it.” - Wendy Lee, writer
For two years I’ve collected the stories and suggestions of dozens of patients and carers such as Wendy Lee, who have survived and even thrived in the NHS.

They form the spine of a book, Staying Alive - How to Get the Best from the NHS, and I’ve included stories from those who suffered very poor care and want to prevent it happening to others.
The contributors came from different backgrounds, and the tough choices they made in their everyday lives served them well when making tough choices about healthcare.
But what struck me most was how the same principles apply to getting the most from life and getting the most from your NHS care.
What keeps us well
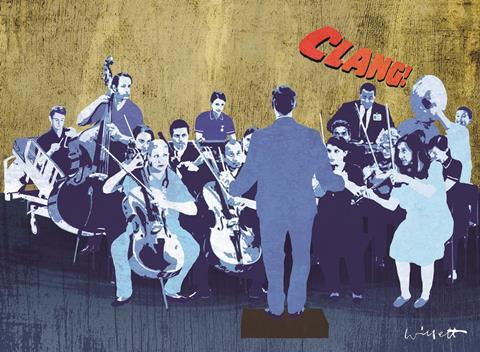
In 2008, the government’s Foresight project reviewed the evidence for what keep us mentally well, and came up with CLANG:
- Connect with others and gain the emotional ballast of being part of a community.
- Learn and feed your curiosity.
- Be active every day in mind and body.
- Notice the world around you and discover the joy of being as well as doing.
- Give back to others.
The happiest people intuitively CLANG but if you struggle for meaning and purpose then it’s a useful acronym to wake up to, and has the research to back it up.
Patients who manage to get the right NHS care, and to keep it on track, also do it by CLANG-ing.
Your best chance of getting the right care for you is to try to connect and build good relationships with the people treating and caring for you, and with charities, other patients, carers and online support.
Learn as much about your illness, the choices available to you and the care you should be getting, and be as active as you can in managing and monitoring your illness and in living and staying well outside the NHS.
You need to notice new or worsening symptoms, observe your treatment and speak up if you have any concerns or questions.
‘If you struggle for meaning and purpose CLANG is a useful acronym to wake up to’
And you need to give back to those caring for and treating you, to the NHS and to other patients so they can benefit from what you have experienced and learned.
Being ill isn’t easy. Almost everyone hates the restrictions it places on their lives, the loss of control and the dependency on others.
Illness can take up all your time, especially if you have to combine being ill with navigating the complexity and chaos of any healthcare system.
The NHS has a £30bn black hole in its finances and is stretched to breaking point. And the more you learn about medicine, the more unsettling it can be.
Seventy per cent of what we can do to prevent disease, and prevent it getting worse, is down to the way we live – medicine contributes a modest 30 per cent.
Many investigations and treatments are of marginal benefit and the evidence on which they are based is poor. For the majority of symptoms, you may well be better off with a dog than a doctor.
Get savvy
A savvy patient knows that an initial diagnosis may not be correct. Ask: “What else could it be?” and “how would I know?”
If the diagnosis is right there will be lots of treatment options, so keep asking:
- “How likely am I to benefit from this test or treatment?”
- “What are the risks?”
- “What is most likely to happen if we just wait and see?”
Often you would live as long as you would have without it. Don’t rush decisions if you don’t have to.
‘I hope it’s the start of a bidet revolution in the NHS. From the bottom up’
A simple list of pros and cons, and some friends to bounce them off, may help you arrive at the right answer for you.
What we can do for ourselves may be more powerful than what the NHS can do for us. The one thing I’ve learned from this book is that patients gain enormously from helping other patients.
I hope it’s the start of a bidet revolution in the NHS. From the bottom up.
Dr Phil Hammond is a GP, journalist and broadcaster. His book Staying Alive - How to Get the Best from the NHS will be published on 2 April


























9 Readers' comments