Ashford and St Peter’s Hospitals Foundation Trust has developed a programme to reduce inpatient stays and improve the discharge process, say Mark Hinchcliffe and Chris Bradley

Inspired by an article in HSJ in 2012 and the Ready to Go guidance issued by the Department of Health in 2010, Ashford and St Peter’s Hospitals Foundation Trust set out to develop a programme aimed at achieving two things:
- a significant reduction in length of stay for inpatients;
- the development of a sustainable and scalable approach that could be used trust-wide.
The programme, the trust’s own version of Ready to Go methodology, aimed to understand the real reasons why patient discharges were being delayed and then set about making simple changes on each ward to reduce these delays. Each ward undertook four steps:
- Understand the biggest delays. Undertaking data capture twice a day identified all delays, on every bed in the ward. Even discharge delays that were previously thought of as “normal”, such as waiting for prescriptions, were recorded.
- Investigate one problem in greater detail. Find the causes of the delay. Teams were encouraged not to stop until they were confident they had found the underlying root cause.
- Identify specific changes to reduce this delay. Once the root cause had been identified, the solutions were usually apparent, although engagement with all staff groups was key to ensuring the solution worked for everybody.
- Use “plan, do, study, act” (PDSA) cycles to implement changes successfully. Only after multiple iterations did an idea develop into a sustainable and long term answer to the problem. Sometimes trials failed at the first attempt, but the teams remained confident, learned from the results and improved the solution the next day.
Improvements made
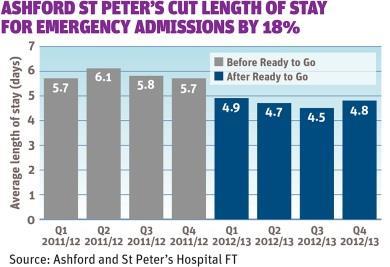
Impressive results were seen across all wards that undertook the programme. Overall, a 15 per cent decrease in length of stay was achieved, across five wards, just eight months after the project launch in May 2012.
Even more encouraging was the fact that the trust’s overall length of stay for emergency admissions in 2012-13 was reduced to 4.7 days from 5.8 days the previous year.
Other benefits included:
- improved ward communications through more regular and more effective board rounds;
- more widespread use of “nurse led discharge” where appropriate;
- improved “in-reach” of consultants to the short stay ward;
- improved visibility of bed availability in rehabilitation wards; and
- improved discharge letter writing and prescription turnaround time.
Key success factors
First, the programme was designed to be sustainable from the start.
The project was split into distinct phases with specific objectives, each one building on the last.
- Phase 1 An externally led team, working across two wards, set out to achieve a reduction in length of stay and develop a set of Ready to Go tools. The programme was also linked directly to the trust’s strategy and headed by the director of nursing, demonstrating the highest levels of organisational commitment.
- Phase 2 A local team worked alongside the external consultants with three further wards, using the new tools. Improvements were made, and then a rollout strategy was identified to bring Ready to Go to the rest of the trust.
- Phase 3 Led entirely by the trust’s team, and involving more wards, changes were made to the discharge governance structures, thereby embedding the changes into daily hospital life.
Although in the short term this programme relied on external expertise, its long term success and sustainability depended on individuals within the trust. The team was not only engaged to deliver change in specific wards, but to build the capability of individuals in the trust to deliver change across the hospital.
Second, staff were encouraged to reinvent the wheel
The programme team decided early in the project that directly imposing solutions would likely be met with resistance as it would not address the issues specific to each ward.
‘Each solution was fully supported by the team who would be using these new ways of working’
Instead, a more collaborative approach was adopted where staff were encouraged to work together to find their own solutions to common problems.
From the outside, it might have seemed that the success of the project resulted from little more than adoption of best practice. However, allowing each ward team to “reinvent the wheel” was exactly what was needed to identify solutions that would work for them. This tailored approach meant that staff engagement was high, and each solution was fully supported by the team who would be using these new ways of working.
Third, data collection was simple and direct
Allied to the principle of engaging with those delivering the service, it was the ward teams who collected the raw, primary data. Care was taken to ensure that data was simple to record because it needed to fit into a busy ward schedule.
Collecting delay data at the ward level meant that each team unearthed their own problems. This way, the ward staff had complete ownership of their data, a deep understanding of some of the root causes causing delays and a shared objective to find solutions.
Mark Hinchcliffe is programme office manager for Ashford and St Peter’s Hospitals Foundation Trust; Chris Bradley is a healthcare consultant
Downloads
Length of stay
Excel



























1 Readers' comment