Dyson Technology aims to engage and educate people about air quality and develop new air purifiers that can further help improve air quality in homes and public spaces, including healthcare settings.
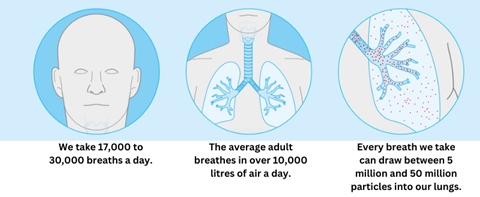
A convincing body of evidence exists linking exposure to outdoor air pollution (a heterogeneous mix of particulate matter, oxides of nitrogen, and ozone) to morbidity and mortality from cardiorespiratory disease and lung cancer. Furthermore, data from a growing number of studies suggest a negative influence on a broader number of diseases including neurodevelopment deficits, dementia, adverse birth outcomes, and diabetes. The magnitude of the problem has recently been endorsed in the updated World Health Organisation Global Air Quality Guidelines, which recently recommended substantially lower air quality limits for PM2.5, PM10 (PM less than 2.5 and 10 μm in diameter respectively) and nitrogen dioxide.
Associated with
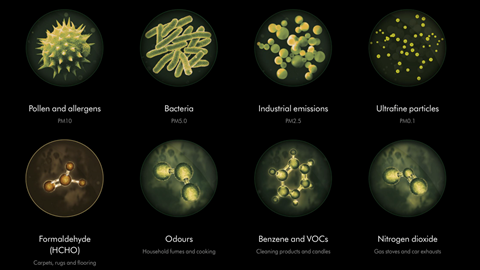
Until relatively recently, air pollution was deemed to be an outdoor hazard, in the general belief that an inside space, be it a home, commercial building, or a public facility, offered protection. Indoor air however is a highly complex cocktail driven by emissions, ventilation, and a rich set of chemical transformations. It contains numerous sources of air pollutants such as human activities (e.g. cooking, heating), products used inside (e.g. cleaning and personal care products), living organisms (e.g. flowers and plants, mould, pets) as well as outdoor air pollutants that penetrate buildings through cracks, windows, doors, and mechanical ventilation. We also know that ill-health, including the severity and/or prevalence of asthma, is heightened by many indoor air pollutants, including NOx from gas cooking, cleaning products, formaldehyde, and allergens.
Healthcare facilities must also deal with polluted air coming in from the outside where emissions from road traffic, including hospital parking facilities
Healthcare settings are particularly complex and sensitive environments. While their primary purpose is to promote, restore, or maintain health for everyone, they are high-risk spaces. They accommodate many different activities and a high density and flow of users that differ in terms of their health status. Patients for example include people who are disproportionately affected by air pollution, even at low concentrations, such as children, the elderly, and people with a lung or heart condition who often have to visit and spend long periods of time. Yet air quality in hospitals and other healthcare facilities can be a significant risk factor owing to the presence of pollutants that are often at higher concentrations compared to other indoor spaces. Furthermore, the provision of a round-the-clock service by hospitals means there is no idle time to recover from emissions and the consequent impact on indoor air quality.
Sources of poor IAQ within clinical environments include building and decoration materials, furniture, and furnishing containing formaldehyde and other volatile organic compounds, cleaning, disinfecting, and sterilising practices employing fumigants, medicines, and medical procedures that use chemicals such as hydrogen peroxide and polymer materials that emit phthalates and high numbers of people arriving and leaving. Pathogenic microbes are also suspended in the air, enabling disease to be transmitted through coughing, sneezing, and talking by infected patients, staff, and visitors. As a result, the indoor air contains a complex mixture of chemical, particulate, and microbiological compounds. Staff, patients, and visitors are sources of microbial spreading and also vulnerable to be infected. As a consequence, cleanliness is non-negotiable, with hygiene measures and infection control policies being stringently observed. With that comes elevated concentrations of harsh cleaning chemicals and increases in humidity that can lead to the growth of mould. The direct emission of chemicals during disinfection is complicated by a wealth of predominantly uncharacterised chemical transformations through which secondary pollutants can be formed that further react to form other potentially harmful species. Furthermore, mechanical ventilation systems often used in clinical settings can not only resuspend bioaerosols, but also contribute to the development of bacteria and mould spores in air filters if they are not properly maintained. Indoor air quality also become worse owing to a building’s age and condition.
Improper control of hospital IAQ may cause hospital-acquired infections and work-related respiratory diseases
Healthcare facilities must also deal with polluted air coming in from the outside where emissions from road traffic, including hospital parking facilities, and generators employed to prevent power interruptions represent a further threat to IAQ. In 2019 a British Lung Foundation study revealed that 2,220 GP practices and 248 hospitals (1 in 3 GP surgeries and 1 in 4 hospitals) in England were in areas where outdoor PM2.5 concentrations exceeded the then WHO recommended average annual levels of 10 µg/m3 (the revised 2021 WHO guideline value for PM2.5 is 5 μg/m3). More recent data published by City Hall earlier this year showed that every hospital and medical centre in London is in an area exceeding the current WHO AQG for PM2.5.
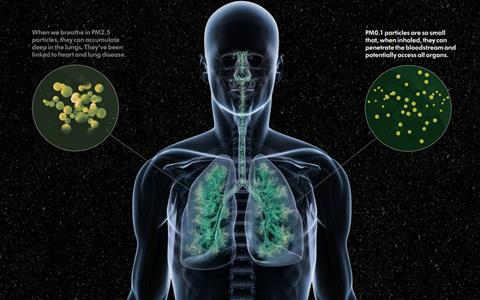
Headaches, fatigue, dryness, and irritation of the eyes and skin are common complaints of healthcare professionals that have often been attributed to poor air quality. Indoor air pollutants may also worsen the health of susceptible patients with pre-existing disease. More seriously, improper control of hospital IAQ may cause hospital-acquired infections and work-related respiratory diseases.
The assessment and management of this invisible danger in all areas of healthcare facilities, including outpatient halls, waiting rooms and cafeterias, is of utmost importance for patient safety and occupational health. Complex environments require specialised programmes to:
- effectively monitor IAQ
- control emission sources
- coordinate preventive activities
- promote public awareness through engaging and high-quality educational materials
The scientific community should continue to investigate the issue, define smart and efficient procedures and design monitoring protocols and tools to strengthen and improve mitigation measures so that the air is safe for staff and patients to breathe.
Dyson Technology Limited continues to investigate air pollution around the world. Air quality monitoring backpacks, developed by company engineers and scientists to collect air pollution data on the move are being used in the Achieving Control of Asthma in Children In Africa study led by Queen Mary University London and Imperial College London. This initiative aims to describe personal exposure to air pollution in urban children with asthma symptoms in sub-Saharan Africa. The backpacks have also been used in studies with athletes in Australia, Germany, Japan, the Netherlands, Russia and Switzerland and schoolchildren in the UK to evaluate personal exposure to air pollution and how to avoid it. Dyson is using these relatable initiatives as a tool to engage and educate people about air quality and is applying the research to develop new air purifiers that can further help improve air quality in homes and public spaces, including healthcare settings.


























