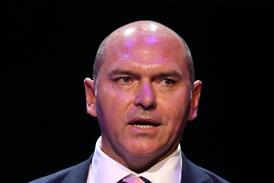
The deputy medical director of NHS England said it would only close a GP practice if it was “at the extremes of immediate public safety”.
In a HSJ interview Mike Bewick said the national body had “been working with CQC to make sure there are some appropriate responses available when major deficiencies are found” so it is “not coming into this completely in the dark”. The Care Quality Commission’s first 1,000 general practice inspections found major concerns in nine surgeries.
Although practices must be registered with the CQC, Dr Bewick explained NHS England had “overall governance” over them, given that it commissioned and contracted general practice. If a CQC inspection found a practice was not fulfilling its contractual obligations, NHS England had the right to remove that contract.
He said NHS England would “very rarely” close a practice with immediate effect. “It would have to be at the extremes of immediate public safety. The majority of time it would be about working with those practices very quickly to mitigate and remediate the situation,” he added.
However, “if we felt a doctor wasn’t safe” or “if there was a clinic, if there was a single handed or two partner practice where the medicine was poor, we would immediately look to replace that” with another provider, he added.
NHS England area team directors would decide whether to close a practice, advised by commissioners, and the area team medical director, Dr Bewick explained. They would examine background information on the performance of a practice, staff turnover and whether it retained doctors to decide whether it remained viable.
“It’s a very difficult decision to make”, he said. “You would want to be sure that there was nothing you could put in place to make a change that would continue to allow practice from where patients are expecting to get the delivery of their care.”
The Keogh review into trusts with high mortality rates recommended those placed into special measures were buddied with more successful trusts. Dr Bewick said he “could conceive” something similar for practices with “multiple problems” but there were “no immediate plans” for such a move to be implemented.
From the first wave of GP inspections, a third of practices were found to be failing in at least one essential standard. Dr Bewick said he would expect area teams to write to any underperforming practices outlining the information the CQC had passed on.
“They have to be held to account on this. It’s not something they can ignore,” he added. “The CQC themselves will wish to go back to those practices to re-look, but the area teams would expect them to come up with an action plan, what mitigating actions they’re taking before definitive action be taken and what assistance and help that they might need from commissioners to help them fulfil that.”
He acknowledged there were some “able people working in circumstances not of their own making”, pointing to inequalities in funding and infrastructure across general practice which were a “legacy” from primary care trusts.
He said NHS England was looking “addressing how we move capacity where it is most needed” which he hoped will come though the better care fund (formerly known as the integration transformation fund). He also said NHS England needed to look into how it commissioned primary care in the future.
He admitted “these are pretty slow processes” and it is the “decision for area teams to make, not for us centrally” about whether a practice with multiple problems is remediable in the immediate term.
Dr Bewick said NHS England was “learning” from the inspections. “If we find better ways to work with CQC to commission more effectively, we will help practices proactively get in a better position.”


























5 Readers' comments