System leaders wondering how best to support their primary care networks should take a population health management approach, argue health consultants Dr Simon Munk, Dr Steve Laitner and Toby Lambert.

Sponsored by
As system leaders consider how best to support their local PCNs to meet the requirements of the NHS long-term plan, we would suggest that taking a population health management approach is part of the answer. This involves focusing on which groups in local communities could benefit most from integrated care and support. We find the grid below a useful tool for considering the needs of different groups of people.
Using the table
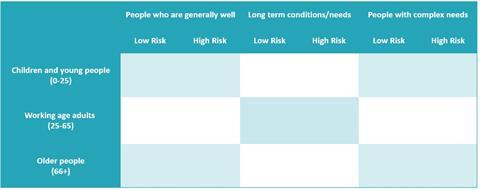
*Risk of progressing to the right with increasing levels of need and care activity
Source: Dr Steve Laitner and Dr Mark Davies, NAPC
People in the left two columns, who are generally well or with one or more long-term conditions, but without complex needs, are usually managed by their GP and practice nurse, with some support from the wider practice-based team and on occasion from hospital or community services. In contrast, it is the people in the right-hand column, those with a complex mix of physical, emotional, and social care needs, sometimes with functional impairment or disability, who require a different sort of highly integrated, proactive and holistic model of care. They will include, children with complex needs and disability; frail older adults with dementia at the end of their life; and adults with severe and enduring mental health, drug and alcohol and social challenges.
Seven steps
Taking such a population health management approach, would allow PCNs to take a leadership role in considering which population groups would benefit most from multidisciplinary team working. This approach typically involves seven steps, each of which require support from the wider system:
1. Engage local stakeholders
Engage colleagues in the PCN, wider stakeholders, public and patient leaders, from the beginning, in agreeing priorities, co-designing and co-delivering new models of care.
2. Consider the care needs of different groups
Work with local stakeholders, using the 3x3 grid, to understand the different needs and numbers in the various population cohorts in the community. Development of an integrated, patient level dataset is an important enabler here.
3. Understand where quality of care, workforce experience and outcomes are poor
Review the data and use the 3x3 to engage your stakeholders in understanding which groups of people currently have poor outcomes and where joined-up working could be better for patients and for the staff working in different services. Agree with stakeholders across the network which specific groups of people to initially prioritise.
4. Improve services and support
Review what support and services these people currently receive for their range of health and care needs and consider how this could be improved. Specifically consider what support could be provided by a multi-disciplinary team working at a PCN level. Consider the assets of the local community.
5. Joined-up working
Consider what can be done to support joined-up working across professional groups and with non-statutory services. This is likely to include care co-ordination/case management, care and support planning, rapid response, joint training and support for professionals and use of trusted assessor models where any member of the MDT carries out an assessment of holistic needs on behalf of the team.
6. Address barriers
Consider the current barriers to delivering joined-up care. This frequently includes a lack of trust between professionals and with others and challenges around sharing data and accessing patient records between organisations. The wider system has an important role to play in supporting inter-organisational working through both providing organisational development support and developing joint care records.
7. Measure impact
Put in data collection mechanisms to measure the impact of better, joined-up care. Measuring whether patients with complex needs are more likely to achieve their priorities and have a seamless experience of care can be a great start. Looking at workforce experience and activity across the system is also often required.

Dr Steve Laitner is a GP in Hertfordshire, who led NAPC work on population health management, and is a clinical associate at CF, healthcare management consultancy and analytics firm.

Dr Simon Munk is a consultant and medical clinician at CF.

Toby Lambert is a partner at CF.
Find out more:
1. Ham C et al. Where next for the NHS reforms: the case for integrated care. London: The King’s Fund; 2011. Available from: https://www.kingsfund.org.uk/publications/articles/where-next-nhs-reforms-case-integrated-care


























