West Hertforshire Hospitals Trust has been running a fully integrated, virtual consultant delivered triaging service that can be a vital part of the armoury against covid-19, say Rama Vancheeswaran, Matthew Knight, David Evans, Michael Van der Watt, Alex Newland Smith, Charlie Oliver, Philip Kelso, Chantoy Spencer and Andrew Barlow

NHS waiting times and targets were all creeping up by the end of 2019 due to increased demands, lesser resource including staffing and more expensive and complex interventions (Findlay, HSJ 2020). The covid-19 pandemic has started to stretch the NHS to its breaking point.
Northern Italy and Spain with higher ITU beds and healthcare staff per patient have nearly collapsed, making the predicament of the NHS even more critical.
Most trusts and primary care organisations have taken unprecedented action, ceasing all elective and outpatient work, leaving patients with already existent comorbid conditions isolated at home suddenly with minimal routine follow-up care.
Destabilisation of these conditions places the patients at increased risk of emergency department attendance and covid-19 infection where there is a significant likelihood of fatal outcomes.
Primary care is valiantly trying to provide remote, telephone-based consultations for its existent patients that were looked after in hospital clinics. Most of these consultations are not face-to-face and without supportive specialist care or investigations.
NHS hospital beds are now mostly occupied by patients with covid-19 infection with longer times in hospital due to infection risk to families or carers and severe presentations. Hospital care is further impaired by 30-40 per cent lesser staffing due to self isolation policies where screening to allow staff back is still awaited.
Personal protective equipment globally is in short supply for all hospital, primary care, social care, ambulance and all allied healthcare workers, further increasing staff sickness. Finally, hospitals are now seeing exhaustion of oxygen supplies as patient needs outpace availability (HSJ, April 2020).
Technology and innovative solutions to reach and treat patients at home are urgently needed to help look after the large number of unwell infected patients with mild to moderate covid-19 who can be managed at home with some supportive care and close observation rather than hospital admission.
Virtual hospital
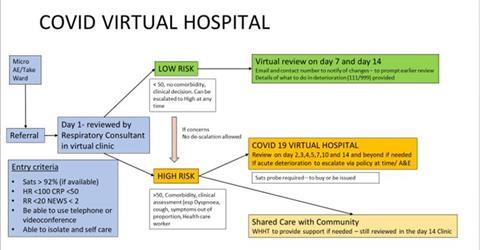
Watford’s virtual hospital uses healthcare workers including consultant staff, respiratory physiologists and physiotherapists not involved directly with the front-line care to enable a specialist model allowing admission prevention or early discharge aiming to reach patients with specialist care at home. The service has been supported by a medical administrative team and volunteer medical students.
By enabling easy referral from acute medical teams, ward teams and accident and emergency department, referrals can be rapidly made. Patients with risk factors for deterioration (age, comorbidities or concerning symptoms) receive oxygen saturation probes to facilitate home monitoring.
Patients are reviewed remotely by phone within 24 hours of referral and triaged into high or low risk follow-up groups. As well as assessing the patient results from blood tests and imaging, they are reviewed to ensure that all results have been appropriately acted upon, recognising that whilst the acute pathways are under extreme pressures the earlier discharge of patients before all results have had senior review can be made safe by ensuring that a senior review occurs promptly after discharge.
Low-risk groups are followed up on day seven and 14 (with safety netting advice) and high-risk groups followed up daily for the first five days and then on alternate days until day 14. General clinical symptomology is assessed and where applicable saturations and pulse collected.
Most consultations so far have occurred to date by home as this was quicker and widely acceptable, although more complex consultations and assessments have occurred via the Attend Anywhere Telemedicine service.
Outcomes
- 393 patients referred in first 21 days of operation
- 32 patients needed subsequent reattendance to hospital – 20 for less than 24 hours, four for less than four days, eight still admitted at the time of writing.
- 266 (67 per cent) patients were triaged as high risk (all readmissions/attendances were from this group)
- 121 patients have been discharged back to primary care – the rest are under current monitoring
- Current capacity (with a 2/3 high risk 1/3 low risk split) is 560 patients (assuming 40 new referrals per day)
Where other pathology has been identified appropriate onward investigations and referrals to speciality waiting lists have been arranged (depending on urgency). The most common finding to date is abnormal radiological imaging not secondary to covid-19 requiring onward follow up.
The capacity of this model of care is to be enhanced by collaboration with local primary care who will take over the management of lower risk patients, again utilising oxygen saturation probes where required.
Under the current circumstances it is difficult to comment upon how much ‘time in hospital’ has been saved by this scheme.
However, we estimate that on average at least one complete day has been saved for all of the high-risk patients and approximately 2-4 hours in the AAU department for each of the low-risk patients (in addition to follow-up visits). This equates to 290 bed days saved over a 21-day period (approximately 14 beds at any one time).
Conclusion
The covid-19 virtual hospital is a small but vital part of the armoury against covid-19. It offers patient reassurance and safety, good clinical care and safety netting, appropriate escalation and readmission pathways and a means to reduce bed occupancy at a time of crisis.
We are working to enhance this model of care with the utilisation of mobile applications to allow the collation of observations to better highlight day-to-day patients most in need of virtual appointments – this will allow us to expand the service enabling clinicians to focus on the patients most in need of input whilst providing appropriate care for all.
Further use of telemedicine platform will facilitate better assessment on the first consultation.
Looking towards the future, we hope to build upon this model in the post-covid-19 recovery period to enable us to assess and manage the large backlog of outpatient referrals that has already started to accumulate due to the cancellation of outpatient clinics – increasing the reach of secondary care to patients in the community and more closely integrating with primary care.


























3 Readers' comments