Hasty implementation of clinical infection services will result in a reduced quality of service to patients with attendant risks to the public. The British Infection Association urges colleagues to share safety concerns with local boards and commissioners, says Tony Elston
The clinical services committee of the British Infection Association represents medical microbiologists in Britain. It contains regional representatives and meets to discuss pertinent current issues.
Infection services are a vital and integral part of all hospitals; they also play an important role in supporting primary care.
‘Good infection prevention and infection services improve the quality of patient care’
Thirty-five to 40 per cent of hospital patients are receiving antibiotics every day and 80 per cent of all antibiotic prescriptions take place in primary care.
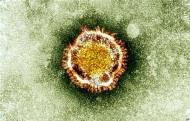
Infection services are the forefront of the battle against antimicrobial resistance, which is a key national and international priority. Infection prevention and control is heavily reliant on the infection service; good infection prevention and infection services improve the quality of patient care.
- High infection rates ‘unacceptable’, says NICE
- Trust cleans up its act with innovative audit tool
- Hunt safety plans ‘will require frontline investment’
- More primary care news and resources
Post-Carter
Committee members and constituents have been involved in the development of infection services since the recommendations of the Carter review of pathology services in 2008.
The report recommended the creation of pathology networks to address issues of capital underfunding, poor infrastructure and staff shortages in various degrees in England.
The report suggested that revenue savings of up to 20 per cent could be realised and that these should be reinvested in the service. Devolved nations are also implementing the advice of the report.
Infection services have welcomed the opportunity to improve their offering but the committee is aware that this process is not without risk. Some developments have taken place that the committee is aware have adversely affected the quality of laboratory services and may have had a negative impact on patient care.
‘The opportunity to improve infection services is not without risk’
We would welcome evidence that these changes do realise benefits to patients and financially.
In networks where infection specialists have been closely involved in designing and implementing change, progress has been made including fit for purpose IT systems, investment in technology, and extended service provision in time and techniques. Many of these have also taken place in the absence of networks.
The ‘hub and spoke’ model
Issues of concern to the committee have arisen where projects have been rushed and/or do not closely involve a range of local professional experts. Several recurring themes have emerged.
A lack of a common IT system across a network has resulted in difficulties with service delivery including significant reporting errors. In particular, clinicians working in satellite or “spoke” hospitals are unaware of results that have a direct impact on clinical care.
Insufficient transport links between spokes and hubs has resulted in increased turnaround times from request to result. Spoke units enjoy a less flexible and nimble service with measurable quality reductions. For example, a norovirus testing service in a spoke laboratory site has been lost as a consequence of centralisation.
Colleagues working in spoke units report spending a significant amount of time trying to access hub staff to deal with queries on specimens from spoke patients.
‘Despite reassurances about safeguards for whistleblowers, colleagues remain reluctant to make these concerns public’
The direct interaction between consultants and their BMS colleagues represents a significant beneficial addition to the processing of specimens that may have been unrecognised and quantified.
We are especially concerned that the soft intelligence which is garnered by working closely with BMS colleagues and scrutinising reports for validation may be lost; the early emergence of novel antimicrobial resistance patterns or the management of outbreaks are two examples that we cite.
Feedback from some colleagues in spoke laboratories is that they have failed to see any benefits post-centralisation. This includes a lack of financial return as demand management and streamlined testing algorithms have been lost.
The committee is aware that despite reassurances about safeguards for whistleblowers, colleagues remain reluctant to make these concerns public.
We are also aware that in a number of potential networks a significant amount of time and effort has been expended only for the venture to collapse as managerial imperatives in the participating hospitals change.
This has hugely reduced morale in the wider microbiological community; this is a fragile and extremely valuable commodity that the country cannot afford to lose. The success in tackling healthcare acquired infections and emerging infectious diseases bears testament to the importance of an effective microbiological service.
Don’t forget the safeguards
In conclusion, the committee welcomes the opportunity to develop infection services.
However, it is concerned that unless safeguards are put in place the hasty implementation of projects will result in a reduced quality of service to patients with attendant risks to the public.
These safeguards should include: full involvement by all local consultants; a sound single IT system; and appropriate transport links between spokes and hubs and communication systems that are able to replicate the efficiency of communication within a self-contained unit.
Without these safeguards we would urge colleagues to share their safety concerns with local boards and commissioners.
Dr Tony Elston is FRCPath consultant microbiologist chair of the British Infection Association’s clinical services committee


























No comments yet