Innovation is often stifled by inward looking, risk averse systems and politics. It is our collective job to recognise patient driven innovation help it to flourish, write Victor Adebowale and Henry Kippin
Shifting power, encouraging resistance, collaborating against the odds and making change all happen against the grain.
‘Shifting power and encouraging resistance happens against the grain’
Are these all characteristics you would associate with the health service? Sometimes, but more likely at the margins.
At an invigorating event hosted by Collaborate and the Social Innovation Partnership last month, four leading lights in the health world called for these traits to be pushed into the mainstream of a health and care system realigned around a richer articulation of our needs, wants and resources as citizens.
- Help us find the top innovators in healthcare
- Spreading innovation: AHSNs step up to the challenge
- David Oliver: Beware the false solutions to the NHS’s challenges
- Sign up to the weekly innovation newsletter
History repeating
There are, we heard, real limits to system change from the top down.
That won’t surprise NHS watchers or anyone even mildly interested in the early results of Andrew Lansley’s attempts to liberate the NHS.

It is partly because structural schisms within the system run deep.
As Stephen Dorrell noted, himself recently liberated from an influential stint as chair of the Commons health committee, history repeats itself, market management remains patchy and political decisions made generations ago have created some fundamental and artificial boundaries that render joined up service provision such a difficult nut to crack.
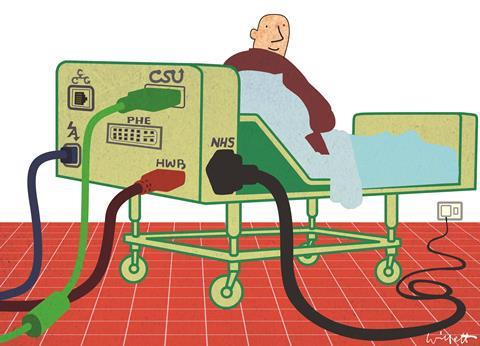
We don’t need another post-mortem – Nick Timmins, a senior fellow at the King’s Fund, has already done a fantastic job – and health secretary Jeremy Hunt’s shift towards patient focus feels like a welcome distraction from acronym laden conversations about the transition from SHAs (strategic health authorities) and PCTs (primary care trusts) to CCGs (clinical commissioning groups) and HWBs (health and wellbeing boards).
However, and this is a big however, there is a long journey from rhetoric to reality on patient engagement.
There is a system disruption to manage before engagement becomes culture change.
‘There is a system disruption to manage before engagement becomes culture change’
And, from what the experts tell us, there is a great deal of learning to be done on how to plug what our recent research called the “collaborative citizen” meaningfully into commissioning and delivery models.
Until we knit this journey together, community led, “socially” driven healthcare will remain the aspiration of relatively powerless advocates in the face of a solidly institutionalised and professionalised NHS.
Which, by the way, is not a critique of why this exists today, but a pretty consensual vision of where healthcare needs to go in the face of massive demand and constrained supply.
Making fresh perspectives possible
So in lieu of a collective awakening of Copernican proportions, what can be done by those believing that a different way is possible? Here’s what we heard:
Collaborate
Do it across sectors, across services, and on behalf of citizens.
Do it in spite of systems and traditions if necessary, and reinforce it with an emerging, but increasingly valuable, evidence base on the things that can be achieved on the demand and supply sides with an integrated local approach.
Engage like you mean it
Listening is indeed in the ear of the beholder.
We seem to be very good at turning passionate views into reinforcing mechanisms for the status quo; yet different approaches are possible when commissioning is used as a proper platform for action and a lever for collective change.
Don’t wait for policy frameworks to catch up
Trial, prototype, learn, share and move forward.
Do it collaboratively and find the mix between clinical innovation and a managerial approach that is more humble, more outward looking and cognisant of the mix of dynamics that are needed to sustain “well” populations.
Some surgery to sustain
Can you change a system with these starting points? Who knows.

We have wonderful health and care services that project cost control, quality and equality of access in a way that is internationally enviable.
And rightly so; one only needs to look at president Barrack Obama’s tribulations with the US insurance model or Japan’s efforts to control spiralling costs to realise that in the UK we are lucky.
Many expert predictions tell us, however, that to sustain this service will require some surgery.
Demand and supply challenges will change the shape of the system eventually.
Collective responsibility
The question is how. Changes will be defined by how we accept that cost, scale, volume and a largely medicalised formula for change. If we don’t want a race to the bottom, we need to work out how to embed different models of change, built on social innovation and patient centred collaboration.
As London regional director of Public Health England Yvonne Doyle argued, it is possible and it is happening.
Clinicians, academics, NHS managers, local authorities and care professionals are all already playing a part in places such as Bromley by Bow.
So as the maxim goes, the future may already be here but it is unevenly distributed.
‘The future may already be here but it is unevenly distributed’
Yet participants also told us that diffusion of ideas is hard in the face of system incentives that can create an inward looking and risk averse logic: stifling innovation, rewarding existing over novel practice, and narrowing the art of commissioning in a context where creative ways of meeting outcomes should be king.
It is our collective job to recognise patient driven innovation where we see it, support it and create the space and the relationships for the collaborative citizen to flourish.
Collaborate’s health collaboration lab will be taking on this task from the autumn. We will welcome your input.
Lord Victor Adebowale is chair and Dr Henry Kippin is director of Collaborate, a policy and practice hub established to improve cross-sector thinking, culture and practice in public services. The Health Collaboration Lab will launch in autumn 2014. For more information on Collaborate’s work email Dr Kippin



























1 Readers' comment