The chance to produce an AQP implementation pack offered potent insights into how the service area should develop. Sheena Hennell explains how one PCT cluster went about their project.
The Department of Health has committed to working alongside the NHS to support the phased roll-out of extended patient choice of “any qualified provider”. This roll-out starts with selected community and mental health services from April 2012.
Eight primary care trusts were selected to manage individual projects in order to produce any qualified provider implementation packs for a particular service area.
The project broadly comprised an engagement exercise with patients and public, the writing of an outcome-based service specification, the development of a currency and production of an AQP pack.
Wirral, on behalf of Cheshire, Warrington and Wirral PCT cluster, was asked to produce an implementation pack for a community continence service.
The project plan identified a patient and public engagement exercise to run in weeks one to four, the development of the specification incorporating a process of review and revise over the full 12 weeks, and alongside this, during weeks six to 12 the development of a currency. The final AQP pack was to be completed and presented by week 12.
A project lead, project officer and chair were appointed for the 12 week timeline. Key leads for information, finance, contracting, and medicines management were co-opted and crucially a clinical lead was identified and recruited.
The project team commissioned an external agency to deliver cluster-wide engagement with patients and the public. An engagement brief outlining the objectives, methodology and reporting line with timescales was agreed with the successful agency.
We asked the question: “What would patients and the public need to know to make an informed choice?” and secondly could that information support the development of the continence specification and shape future services? In addition, in what format should the information be presented? Are patients ready for choice and can they make informed decisions regarding care?
Dignity and respect
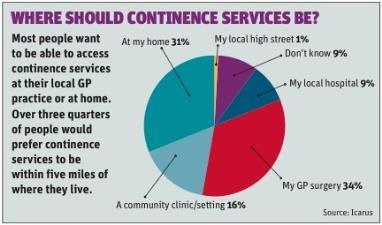
A total of 355 people were surveyed across the cluster by research company Icarus. The results showed that choice of alternative provider was not as high a priority, as many participants wanted the GP practice to be involved in the provision (see graph). GP/patient relationships were held in high regard, with patients recognising the additional benefit of the GP’s knowledge of their condition.
Knowledgeable staff were seen as an essential requirement. In addition, many respondents made it clear that confidentiality, privacy and dignity and respect, were very important when choosing a service.
Patients were in fact concerned for the safety and continuation of traditional NHS services. The research found: “There was a view that commercial operators would be able to ‘cherry pick’ those parts of the service that were most profitable… There was also worry that this might lead in future to an inferior service being available.”
Alongside the engagement exercise, the current local provider and cluster patient engagement team held several focus groups and all views informed the development of the service specification.
Icarus concluded that the value of NHS services could not be underestimated – and neither could the role of the GP.
The project lead took overall responsibility for writing the service specification using both the current local community service specifications and a review of current literature to provide up-to-date guidance and best practice standards. Key stakeholder engagement was vital for success and two groups were formed.
The first was a local, clinical, email engagement group comprising clinical lead, continence nurses, urologists, elderly medicine consultants, gynaecologists and paediatricians who supported the initial building of the specification. This fed into a national multidisciplinary expert reference group to refine and edit the specification.
The specification developed based on the following, and the project lead incorporated a cycle of review and revise using the feedback and comments from both groups:
- local continence expert/clinical lead advice;
- patient and public experience outcomes;
- prevalence;
- use of National Institute for Health and Clinical Excellence and local guidance;
- pathways;
- service model with integration;
- referral forms;
- outcomes and outcome measures.
To develop meaningful outcomes, the group adopted the logic model, which supports the outcome-based element of this specification, focusing on the inputs through to impact. Outcomes must be measurable and are more than just activity.
Commissioners must performance manage services in terms of the effectiveness of intervention relative to the client’s outcome and the wider impact for the health economy. Using validated quality of life questionnaires and a symptom-profiling questionnaire before and after supports this process and standardising this allows for benchmarking and comparison.
Key outcomes were identified as follows:
- satisfaction with the quality of the service;
- number of adults and children cured, treated or symptoms alleviated while within the service or post discharge;
- number of adults and children self managing at nine months;
- key impacts over time;
- reduction in avoidable secondary care attendance, and admission;
- reduction in urinary tract infections;
- reduction in unnecessary treatment and inappropriate reliance on products for the containment of urinary/faecal incontinence.
Currency profiling was undertaken by the finance lead. It comprised identifying current quantum of cost (current service block) and current activity. A modelling process was –undertaken which generated two appointment levels based on complexity, staff banding and time required. The tariffs reflected pathway prices which included both a cap (maximum of five follow-ups) and top-up incentive for achieving outcomes of cured, treated or symptoms alleviated while within the service or post discharge.
The any qualified provider pack was delivered on time and there were some lessons to share. Finance experts as part of the national reference group, for example from other pack areas, would have supported better testing of draft currencies/tariffs. In general, more communication between implementation pack teams to exchange methodologies and experiences would also have been useful.
We want your views
Get involved in Resource Centre by helping us shape the content of the section, contributing your examples of best practice and sending in questions to be answered by our expert columnists.
If there is a topic you would like to see covered in Resource Centre send in your suggestions to HSJ’s Resource Centre with the subject line “key topic”.
Are you part of a discussion in HSJ’s LinkedIn group that you would like to see highlighted in Resource Centre? Let us know by emailing hsjrsourcecentre@emap.com with the subject line ‘LinkedIn”.


























No comments yet