GE Healthcare Partners’ Tim O’Hanlon considers ways technology solutions can help clinicians and patients alike

We are currently being asked by clients to determine if, and how, digital technology can transform care.
For the technology people, the response to the first question is almost always “yes” but for many clinicians and patients the answer is less certain – especially when they move from considering what might be theoretically possible, in the future, to the problems that clinicians and their patients are facing now.
In a recent discussion with a client about the digital disruption of healthcare, a clinician posed the question, “Ah…yes but who wants a dying app?”
The challenge was built upon the following premises:
Will a digital solution ever…
- Comfort a dying patient?
- Clean up the blood in a trauma unit?
- Be the “thing” you turn to at the moment of your greatest despair?
- Solve the breakdown in relationships between health and social care, managers and clinicians?
- Stop an 80-year-old patient arriving at a community care centre at 3am?
The debate continued about the personalisation of healthcare and it being about the “patient within the patient”, i.e. putting a face to the patient and treating them as a person and not just a series of symptoms. It was perceived that a ruthless march towards technology solutions would de-humanise the process.
That got us thinking about the correlation between services and patient needs. Here is an example of how Quality Function Deployment – a simple tool - can be used to ensure that new services, current and new partners are aligned in their work to meet patient needs. In this example (developed by a group of AHPs) the most obvious lack of alignment was continuity of care.
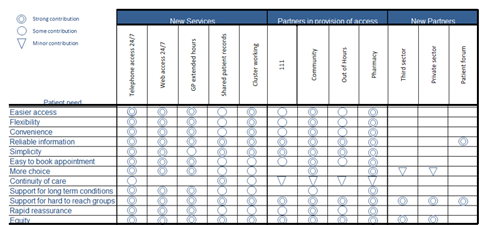
The discussion thus continued as to how could “digital” help? The matrix, above, shows that:
- A shared patient record is a strong contributor to continuity of care.
- New partners had not been fully engaged as contributors to the overall solution.
So; it is possible to identify – in a structured way – how “digital” might best contribute to addressing specific challenges from the perspective of patient needs. However, is it always the answer?
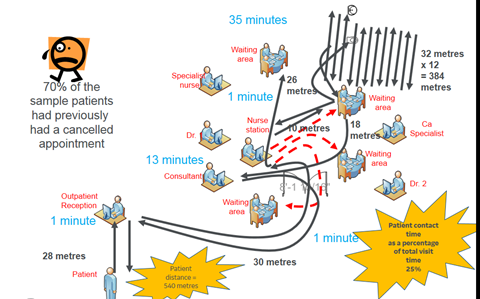
The diagram below shows that a patient attending a urology clinic walked 540 metres – mostly to and from a water cooler to get 7 cups of water for his flow test – and contact time with a clinician was 25% of the total visit time. An app won’t sort that issue but 70% of the patients in that clinic had had a previous appointment cancelled and “digital” could help solve that problem.
Working problem back
Techy people like to invent stuff. Sometimes it is incredibly valuable and sometimes it is not. The “problem back” principle looks, instead, at the issue that needs resolving. Examples of patient experience feedback include:
“I have been here 45 minutes and no one has told me what is happening”
“It’s like being on a crowded bus”
“I waited an hour and half for that..”[3 minutes with the consultant]
“I was already tested in A&E a month ago”
“If I wait any longer, I’ll have to put more money in for the car park”
“Why are you sending me an appointment letter when you have just given me an appointment card”
“We’ve been waiting here an hour now, I’ll go and say something in case we have been missed”
Staff often have similar issues:
“We don’t get time for a break”
“Reps come in and delay the consultants”
“Secretaries delay the consultants”
“Ward/emergency requirements can call consultants away”
“Continual phone calls”
“Not very confidential for the patients”
“When patients go to X-ray and come back they end up with 2 sessions with the consultant and this delays other appointments”
“Patients get delayed because of other patients coming in late”
Is “digital” the answer to all these ills or do we just need someone to make a decision or to do things right first time?
Traditional versus digital
If “digital” is not the only answer, what are more traditional ways of addressing patient experience challenges?
The use of the 6 ’c’s of nursing are an excellent foundation for enhancing patient experience. Techniques such as driver diagrams and the King’s Fund Patient and Family-Centred Care toolkit offer mechanisms for improving patient experience, which are much more about the human interaction than the technological.
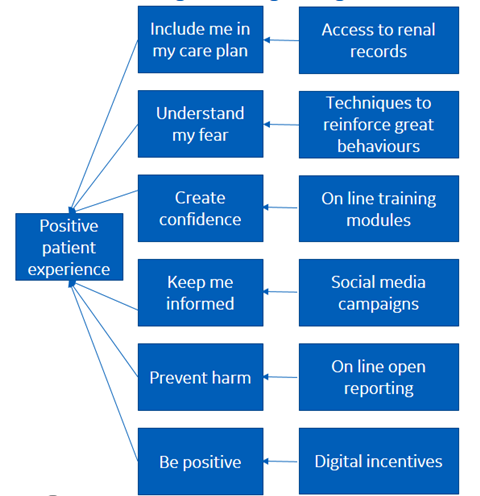
We can, however, also use the same techniques to ensure that “digital” is supporting such efforts. The following driver diagram explores the links between a positive patient experience and “digital” options:
Irrespective of the merits of “digital” disruption, for many patients the preferred option may be to remain a little more traditional for another generation or two. An example is the use of an app at GP surgery level providing access to appointment booking, repeat prescriptions and medical records. For those patients who have mastered the system, it is fantastic but the surgery performs poorly on NHS Choices and shows only 12% of its registered patients taking up the “digital” option.
The development of machine learning, artificial intelligence and vast data capture from “internet of things” devices, offers the prospect of massive opportunities to enhance the decision making for patients. For many portions of our digitally enabled society this will offer new ways of getting to the right care first time and the development of clinical and citizen decision support tools.
We should, however, recognise that any current divide between the digitally enabled and digitally disconnected citizens will be amplified by such technologies and we will need to consider the digitally isolated citizen even more in the future if we are to preserve equality of access to care services.
Ultimately patients will choose what enhances their experience not technologists but the options available to citizens may be limited by their personal digital landscape.
Tim O’Hanlon is partner at GE Healthcare Partners Eastern Growth Markets.


























No comments yet