Every commissioner, provider and professional has a responsibility to provide equitable care. But what happens when people from diverse groups aren’t accessing health services, asks Annie Ford and colleagues
Merton in south west London houses leafy suburbs, is home to Wimbledon and about 100,000 people from minority ethnic groups. In some wards, about one third of the population are from minority ethnic groups. Local audits found that people from migrant communities were least likely to be registered with a GP and more likely to use A&E, even during normal working hours.
People did not know about primary care or out-of-hours services and were living with progressively deteriorating conditions until they reached crisis point. This is not good for people’s health and it is not sustainable for health services.
Barriers to healthcare
People from migrant communities may not use primary care because the services, expectations and payment requirements are very different in their country of origin. They may not feel comfortable communicating in English or they may feel embarrassed about health issues. They may think that using A&E services is easier or more appropriate, without realising there are other options.
Merton Healthcare decided to tackle this issue. Over the past two years, bilingual advocacy services has been set up to signpost people to NHS services, run education workshops and provide interpreting services in GP practices and during home visits. In this time 332 people have attended 22 six-week education programmes run by a multidisciplinary team of health coaches, paramedics, pharmacists, midwives, nutritionists and falls specialists.
Four large education open days were run in community venues to create a friendly environment where more than 400 people attended to ask for advice. We trained 50 professionals on understanding the diverse needs of local communities and the health barriers for migrant people such as those from Eastern Europe and Southeast Asia. The goal was to break the cycle of inequalities and ensure migrant communities had better access to health services.
‘Giving people alternatives has had an impact on healthy lifestyles and on the use of hospital services’
These initiatives have been a huge success and are being rolled out to neighbouring areas. People from migrant communities say they are now more aware of the services and support available, and more comfortable accessing health and social care. And professionals are reporting more empathy and understanding for the diverse groups they are supporting.
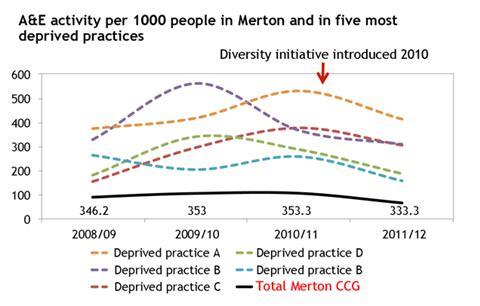
This has led to a change in the use of A&E services. Previously, A&E use was increasing year on year. Now, this is plateauing out and there have been reductions in A&E use amongst the most deprived wards which have been particularly targeted for support.
In fact, the five practices serving the most deprived populations have reduced A&E activity by about 10 per cent. Giving people alternatives has had an impact on healthy lifestyles and on the use of hospital services.
Every area must consider diversity, and each service may provide support in different ways, as appropriate for the needs of the local community. The learning from Merton suggests some top tips, no matter what strategies are put in place.
In Merton, there have been great successes and the initiatives are now being rolled out to neighbouring areas. There is always more that can be done to ensure high quality and accessible services for all.
Tips on targeting diversity
Have strong project managers: People with a solid background in equality and diversity working jointly with people from local communities. Drawing advocacy workers from local communities and giving them autonomy is empowering.
Co-create programmes: Do ask people what they want and see how they can help to provide it. Programmes that are co-created are more likely to meet people’s needs and be sustained.
Seek council member support: Gain support from council members, NHS leaders and community groups early on. Using a simple PowerPoint presentation that focuses on potential benefits in lay terms and tugs at the heart strings makes it easy for funders and other stakeholders to engage.
Research community backgrounds: Do talk to people and research the history and background of local communities. Recognise that some people may have previously had to pay for health services or be scared of government-run services. Looking at statistics can provide insight into local trends, but there is no substitute for talking to patients, carers and community groups.
Recognise subgroups: Do recognise that there are subgroups within hard-to-reach communities. Not everyone from a particular ethnic group, gender, sexuality or disability is the same. People have individual needs. It is not enough to focus on the needs of those who are the most vocal.
Target young people: Do consider how to target young people. Children and adolescents have a key role to play in their own health and that of their families and communities.
Allocate sufficient time: Do allow enough time to build trust. Things won’t happen overnight. The focus is not on achieving targets immediately, but rather on engaging and empowering people to live healthier lives. Timeframes need to be realistic enough to allow programmes to flourish.
Celebrate sucesses: Do celebrate successes and “quick wins”. Every small change is an achievement. Focusing on successes shows people you are making a difference, can maintain staff morale and community momentum and can encourage ongoing funding.
Recruit wider champions: Don’t just rely on one or two people. Champions are important and personalities often make or break the success of initiatives, but motivating a wide team from the outset ensures greater buy-in and sustainability.
Enhance existing services: Don’t be critical of existing services when setting up something new. Demonstrate how initiatives will enhance existing services. Focus on showing people how they can be part of the solution, rather than only highlighting problems.
Delegate tasks: Don’t try to do everything yourself. Helping people to stop smoking, maintain a healthy weight and reduce drinking may be best achieved by working with partners such as social services, local businesses, gyms, schools and community centres.
Involve wider community: Charities and community groups can provide invaluable skills and knowledge, as well as a “way in” to hard-to-reach communities. But it is important to make sure that any tasks handed over to other organisations are followed through so that local communities don’t lose trust or momentum.
Annie Ford is diversity programme manager at Merton Healthcare, Debra de Silva is head of evaluation at The Evidence Centre and Daniel Archer is data analyst at Merton Healthcare























1 Readers' comment