Productivity in the NHS remains markedly below pre-pandemic levels, while trusts are faced with growing demand and increased financial pressure. Public satisfaction has hit historic lows, yet most trusts still lack a clear view of where consultant time is going – and where it’s being lost. In this article, BCG has set out five key success factors crucial for driving a clinician-led productivity transformation built on transparency, equity, and trust.
10.8 million patients are missing vs 2019-20 – but where did they go?
Sponsored and written by
NHS trusts are facing unprecedented financial pressures and persistent backlogs as well as ambitious national targets. Five years on from the start of the pandemic, clinical productivity remains significantly below pre-pandemic levels, while public dissatisfaction with the NHS reaches its highest level since records began. Without strategic, purposeful action to address these challenges, the situation will only continue to exacerbate. BCG analysis estimates there is already a national productivity gap of 10.8 million patients/year across outpatients and theatres compared to pre-pandemic levels.
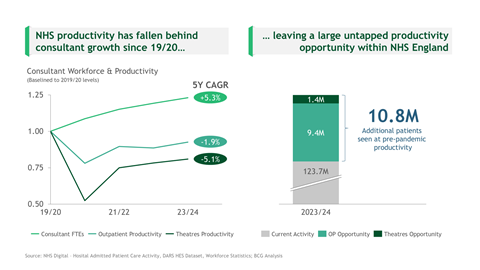
To begin to troubleshoot this challenge, trusts need a clear picture of performance at both a consultant and specialty level, but the reality is most hospitals don’t have access to this. While NHS data remains plentiful across sources such as NHS Digital and Model Hospital, trusts struggle to build a clear internal perspective due to fragmented data across multiple siloed systems.
This is further impacted by inconsistencies in consultant job planning, with many clinicians lacking up-to-date plans and large variation in activity delivery versus expectations. When this data is accessible, there remains little guidance on interpreting it, leaving trusts poorly equipped to identify bottlenecks, support underperforming services, or scale best practices.
So, why don’t people act?
There are three key barriers that mean clinical and operational leaders are hesitant to push for change:
- A lack of visibility on the opportunity for improvement: While the activity data exists, it’s scattered across multiple systems and quality remains inconsistent. Collating it to compare delivery against job plans or templates requires substantial manual effort, limiting its use and credibility in driving action. Without reliable, interpretable data, trusts struggle to surface unwarranted variation or missed capacity, while clinicians remain understandably sceptical of its purpose. Unlocking productivity starts with having the data to see it.
- Productivity discussions will require uncomfortable conversations: Increased oversight can feel threatening in an already strained system. Leaders recognise the need for change, but without clear guidance focused on collaborative improvement rather than punitive oversight, it’s hard to engage teams in difficult conversations about performance. In our experience, this data uncovers consultants delivering both much higher and lower levels of productivity than their plans – highlighting this variation presents an opportunity to help rebalance the load.
- Learned helplessness has eroded operational ‘muscle memory’: After years of unrelenting focus on managing the NHS’s short-term operational pressure, many teams have lost confidence in their ability to drive meaningful change. The reflexes that once enabled continuous improvement – data-driven learning, clinician-led problem-solving, iterating solutions – have weakened. Without support, long-term transformational change feels out of reach.
How to drive change, driven by clinicians
Improving clinical productivity requires more than just pressure – it needs a reimagined system where it is seen as a shared responsibility built on transparency, equity, and trust. These three pillars create the conditions for consistent action, sustained engagement, and meaningful change.
Transparency
- Enable access to real-time, reliable data through automated dashboards to reduce manual barriers and reveal variation
- Make productivity metrics visible at both specialty and individual levels – not to name and shame but to facilitate the early identification of outliers and target support
- Provide clear, interpretable insights that guide conversations and support data-led decision making
Equity
- Empower divisional directors and clinical leads with structured review processes, avoiding bias or exceptionalism
- Identify workload imbalances and act early to redistribute sessions and support fairly
- Create standardised review templates to enable consistent assessment across departments and roles
Trust
- Engage clinicians in the design of improvement approaches so they feel ownership, integrating an understanding of specialty nuances into interpretation of the data
- Focus discussions on collaborative problem-solving – not performance policing – utilising productivity data as a tool for continuous improvement, not a weapon
- Ensure actions are followed through and communicated, reinforcing credibility and commitment
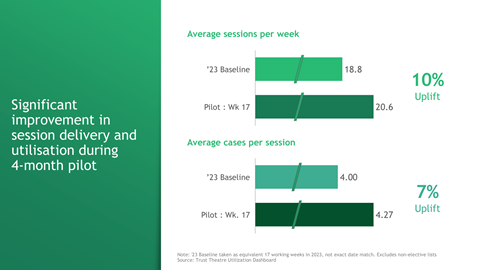
How big is the opportunity to improve clinical productivity – really? Well, our recent work at a large NHS trust indicates it should not be underestimated. Working closely with the ophthalmology department, we identified and implemented several initiatives, targeting increase fulfilment of job planned/scheduled sessions and the number of cases performed per session. This work delivered an 18 per cent increase in patients seen per week in just over four months and crucially this was achieved without any additional funding or staff. These gains, achieved through practical, replicable solutions, demonstrate the real potential of better data visibility, improved planning, and collaborative problem solving.
What is the key to a successful transformation?
From our experience, there are five critical enablers for delivering this effort at scale – each essential to making productivity not just visible, but actionable.
1. Unify efforts around a collective ambition
This transformation must be framed around a shared case for change – rooted not in performance pressure, but in quality, equity, and improvement. A supportive narrative is essential to securing clinical buy-in. Leaders must articulate a clear and consistent ambition: improving productivity is not about working harder, but working smarter, to deliver better care for more patients.
2. Empower clinicians at the heart of change
Productivity improvement cannot be something done to consultants, but something led by them. By enabling clinical leaders to address systemic barriers and freeing up time to focus on patients, trusts can build momentum around meaningful change.
3. Align leadership with clear roles and escalation paths
Divisional directors, clinical leads and general managers need a unified understanding of their roles in the process, how to interpret variation, and when and how to intervene utilising the practical levers at their disposal. When leadership teams are aligned, consistent action becomes possible at scale.
4. Build transparency through trusted data
Trusts must invest in the digital tooling to create reliable, real-time visibility over job planning, and clinical activity delivery. This reduces manual burden and makes productivity measurable, enabling data-led decision-making and informed conversations.
5. Turn insight into action
Data alone isn’t enough. Leaders need structured playbooks, clear metrics and repeatable processes that translate visibility into improvement. When action becomes routine, trusts can embed continuous improvement centred around shared best practices into their operations.
Boldness, not bandwidth, will define the outcome
Improving clinical productivity is not simply about pushing harder but instead enabling staff and creating the right conditions for change. Putting transparency, leadership, and clinical ownership at the centre of productivity transformations, trusts can shift from reactive firefighting to proactive improvement. A restoration of pre-pandemic productivity levels could help clear the backlog within mere years. The door is open, but it requires leaders to be brave enough to step through it.
With special thanks to Joel Cooper.








































