As the NHS faces ever-increasing demand, persistent staffing shortages, and an expanding backlog of care, all eyes are on digital solutions.
Indeed, in the coming years, digital technologies – one of health and social care secretary Wes Streeting’s three shifts and a core part of the 10-Year Plan for the NHS – have the potential to radically reshape care.
However, the current approach of implementing point solutions will not be sufficient. To realise digital’s full potential, the NHS must instead undertake an end-to-end digital transformation across the entire patient journey. That means absorbing key lessons from international frontrunners who are already delivering digital at scale.
Sponsored and written by
From ‘point solutions’ to ‘digital front-end’
NHS trusts and integrated care systems up and down the country have been experimenting with digital solutions to help them manage demand better. Tools, such as online booking, chatbots, records access, and video consultations, have made strides in improving access, triage, convenience, and patient empowerment.[1] But challenges remain:
- Implemented as point solutions: When not integrated across existing solutions, digital tools have a limited view of the patient journey, and a patient-centred approach is out of reach.
- Fragmented technology and duplication of efforts: When, for example, there are multiple vendors for GP consultation platforms within ICSs, technology procurement and platform-related decisions are fragmented, and technology is harder to integrate in the future.
- Insufficient returns: Large digital investments are not panning out. To quote one health leader, “We have already invested in a digital triage offering, and did not get the impact we expected.”
As system pressures intensify, what is needed is a broader concept: the “digital front-end”, a framework where digital tools are integrated throughout pathways to facilitate access, alleviate strain on health systems, and improve patient outcomes.
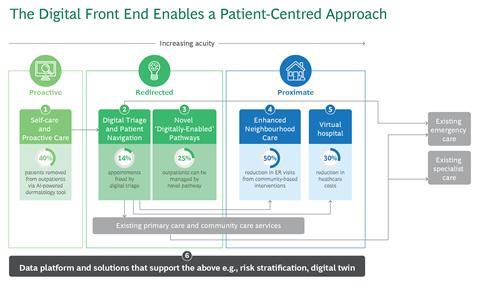
The digital front-end supports prevention, diagnosis, treatment of acute diseases, management of chronic conditions, and recovery. All the tools, from self-care to virtual wards, are connected via a seamless, data-driven continuum. This includes:
- AI-enabled triage and diagnostics (such as dermatology and musculoskeletal pathways)
- Self-care and preventive digital tools
- Remote monitoring platforms for long-term conditions like chronic obstructive pulmonary disease, diabetes, and heart failure
- Virtual wards and “hospital-at-home” models
- Real-time integration with national platforms and shared care records
These innovations are not just tech upgrades. Far more than a sum of its parts, the digital front-end represents a step change to a model of care that is proactive, redirected, and proximate.

How is the rest of the world facing this challenge?
Leading healthcare systems worldwide are increasingly implementing digital front-ends to improve the patient journey. The new healthcare models deliver proactive support for patients at higher risk, embrace novel pathways, and provide care to patients in their communities. These models have already demonstrated value in managing demand.
Denmark: Consistently ranked among the most digital in the world, Denmark has had sundhed.dk portal, a self-help platform, since 2003. Today, the country’s healthcare system is undergoing the most significant overhaul in two decades. It includes a DKK 2bn investment to expand digital solutions outside the hospital and build a national data platform. The goal is to strengthen primary and chronic care, reduce regional inequalities, and improve access to healthcare.
Finland: In 2024, DigiFinland, a special-purpose entity, launched the Finnish national AI ecosystem for social and health services, a network of public, private, and third sectors. Supported by €3m in funding from the Ministry of Social Affairs and Health, the network aims to facilitate the use of AI in social and health services across the country. Healthcare professionals and AI developers from the 200-plus member organisations are working together to create real-world solutions.
Singapore: The National University Health System (NUHS) has designed a “superapp” to engage patients in managing their healthcare. The app, which can be used across NUHS’s 14 different institutions, enables users to manage appointments, coordinate remote care, access medical records, and more. Uptake has been strong, with 1.4 million downloads and 25,000 daily active users in just three years.
Australia: HealthDirect, Australia’s government-funded virtual health service, decided to upgrade and scale the AI-powered clinical decision support system used by its national helpline. After selecting a system that provided the most accurate triage output, HealthDirect launched the solution internally, with the nurses, who provided feedback that was used to improve the solution. The next step was to add AI to the consumer-facing online symptom checker. As a result, HealthDirect has diverted half of its emergency calls to less acute services and granted free healthcare access to approximately 30 million people.
USA: Care provider Ascension Health developed a digital experience that would simplify engagement for both patients and clinicians. Created from the consolidation of data from tens of different EHRs, as well as owned and third-party digital products and data sources, it enables patients to find, manage, and pay for care. The solution was a great success because it focused on both clinicians and consumers. In addition to involving consumers in the product design, the effort included a go-to-market team to lead communications, change management and engage with clinical and operational stakeholders.
Learning from global leaders
Looking at these peers, Boston Consulting Group has identified six key lessons for the NHS:
Set the direction
- Make digital and AI a national priority: Government support in the form of specially designated funding is critical. This means ensuring that there is a tariff for digital pathways to encourage providers to innovate.
- Create a public-private innovation ecosystem: The NHS needs to manage the market more strategically. This may include sharing risk and benefits with the private sector to help drive innovation and scale.
Build in the right way
- Make patients partners in design: Solutions should be co-designed with patients to ensure the tools are patient-centric. There is the potential for patients to increasingly manage their own care – but only if we give them tools that work for them.
- Rethink the workflow to accelerate access and streamline care rather than simply digitising poor paper processes. This also means rethinking how we do things — for example, arranging for tests before sending patients to outpatients.
Deliver the change
- Invest in innovation zones to implement end-to-end, digitally enabled transformation at scale. It is important to pilot strategically and scale rapidly. Focus on only the best use cases and scale pilots quickly to reduce costs.
- Drive adoption and scale through clinician buy-in and change leadership: It is important to involve clinicians in the design process early on and use clinical champions for scaling. The traditional model will need to change so that patients have earlier, better access to specialist advice and diagnostics. That means our workforce will need to change as well.
A call to action
A well-implemented digital front-end solution has the potential to deliver more responsive care to citizens at significantly lower costs, with a shift in care closer to home and reduced workload on services already stretched thin. The NHS’s digital journey is well underway, but to meet today’s pressures and tomorrow’s expectations, it must evolve into an integrated, end-to-end system architecture. The NHS, with a more centralised structure, has a clear imperative and is on the precipice of major change. It has the opportunity not just to catch up — but to lead.
Source
1 Blum, K. (2022). Digital front doors: a deep dive into this growing health care trend. Association of Health Care Journalists.






































