When different organisations with a similar end goal come together, care can be transformed. Salli Jeynes and Bie Nio Ong explain how a partnership was formed to do just that in end of life care
End of life care has moved centre stage not only because of demographic changes and clinical advances, but also because of the renewed focus on quality of care resulting from the Francis report and the review of the Liverpool Care Pathway, among others.

The End of Life Care Strategy and the recent National Care of the Dying Audit for Hospitals, England recognise that end of life care has to be transformed and the End of Life Partnership has been created in Cheshire with the aim of doing just that.
The new partnership is built on three existing work streams that bring a wealth of experience and evidence of good practice:
- Cheshire Hospices Education;
- the End of Life Care Service Model; and
- the Living Well, Dying Well Partnership.
Cheshire Hospices Education was set up in 1998 through St Luke’s Cheshire Hospice in Winsford, Hospice of the Good Shepherd in Chester and East Cheshire Hospice in Macclesfield to provide education and training drawing on their innovative palliative care practice.
This developed into an extensive portfolio ranging from short courses and specialist conferences to university accredited programmes. The courses are flexible and dynamic, and supported by e-learning. Recent validation of the bachelor and masters curriculums by Chester University confirmed they are academically robust and innovative in both content and delivery.
Steps to success
The End of Life Care Service Model was set up in 2010 by local service providers and supported by Macmillan Cancer Support. It provides facilitation and support to care providers and organisations backed up by the EPAIGE website (Electronic Prognostic Assessment and Information Giude for the End of Life Care), which contains a wealth of information for practitioners.
‘The aim is to improve health and wellbeing by supporting change in public knowledge, attitudes and behaviour towards death, dying and loss’
The facilitators work alongside professionals and care workers in their care settings, which include hospitals, care homes and primary care.
As an example, a community “do not attempt cardiopulmonary resuscitation” policy has been developed and put into operation. The team is now working with East Cheshire Trust and Mid Cheshire Hospitals Foundation Trust to develop the policy and support ward, community and care home staff in its implementation.
The team has been heavily involved in the North West’s “six steps to success” programme for care homes, which equips staff to deliver high quality end of life care by using a structured, patient centred approach. The first stage of this programme has been evaluated by Edge Hill University and demonstrated increased confidence of care home staff in assessment, care planning and communication.
- Trusts to be inspected against new end of life care priorities
- Achieve the gold standard in end of life care
- How to provide 24/7, joined up palliative care
The Living Well, Dying Well Partnership, supported by St Luke’s Cheshire Hospice and Macmillan, represents a unique work stream focusing on the public health aspects of death and dying.
The aim is to improve health and wellbeing by supporting change in public knowledge, attitudes and behaviour towards death, dying and loss.Through this we can make living well and dying well the norm.
The team collaborates with a variety of community groups and community champions, statutory and third sector organisations by holding workshops and local events. An evaluation of the process and outcomes of this work by Teesside University is nearing completion.
Integrate work streams
In March the End of Life Partnership was launched, bringing together these work streams and building on their relationships with local communities, workplaces, service providers, commissioners, the strategic clinical network and care workers across different settings.
‘The added value of the partnership lies in being able to integrate the work streams to form a coherent framework’
By pooling and joining up their expertise, overall efficiency, capacity, responsiveness and impact can be improved to help create a more complete and holistic approach to death, dying and loss.
The addition of the research and evaluation arm allows for a systematic gathering of evidence. The partnership is established as a separate charity and intends to:
- reduce duplication of effort;
- maximise and develop partners’ skills; and
- create a more joined up, integrated and outcome driven approach.
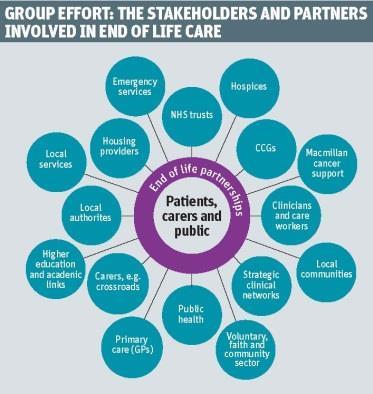
It brings a wide range of organisations together in a strategic partnership executive (see diagram, below) and is financially supported by commissioners, hospices, NHS trusts, Macmillan and a strategic clinical network. It attracts further income through its own education and research activities.

The added value of the partnership lies in being able to integrate the work streams with seven cross-cutting themes to form a coherent framework to which all partners and the board of trustees has signed up (see diagram, below).
Sound strategy
Patients and the public have been involved through the Living Well, Dying Well Partnership community consultations. The research and evaluation team is carrying out a needs assessment with the local authority’s public health department to further focus the three-year strategy and robustly underpin the business plan.
Financial commitment from all partners has been secured and a realistic budget agreed to cover the operation of all the workstreams and the overall management of the End of Life Partnership.
‘We enecourage hospital, primary and community services, care home, hospice and local authority teams to share their assets and skills’
Colleagues, stakeholders and healthcare leaders meet regularly and have signed up to a common, guiding ethos and set of principles. They have fed in, shared and agreed their local and organisational priorities in relation to end of life care. This results in a greater integration of services, and colleagues communicating more easily and readily with each other as they work towards shared goals.
An example of how this joined up approach works is the way in which the new care plan for end of life was developed and introduced.
Using established relationships from diverse organisations, the partnership was able to work with local commissioners, specialists, practitioners and the public to formulate the local care plan for use across all care settings. This was underpinned by a strong educational strategy to ensure the safe and effective implementation of the care plan.
Feeding back
A robust evaluation process was put in place by the research and evaluation team, allowing for a systematic review of the care plan’s operation and its impact on the quality of care and the experience of patients and their social networks.
‘The partnership’s vision goes beyond standards, guidelines and pathways’
New approaches are reflected in different ways of working that focus on the identification of end of life care priorities by multiple stakeholders. These are captured in a coherent framework of key performance indicators, each of which requires partners to work either as a totality or in various combinations, depending on who contributes to the achievement of a particular indicator.
Through these varying and cross-cutting partnerships, organisational barriers are broken down, capacity is built and resources are shared, thereby avoiding duplication of effort and silo working.
The work of the End of Life Partnership encourages and enables hospital, primary and community services, care home, hospice and local authority teams to talk to each other and to share their assets and skills.
Broad vision
When launching the partnership the national clinical director, Dr Bee Wee, outlined her vision of the “house of care”. this goes beyond standards, guidelines and pathways, and emphasises values and principles that drive personalised, coordinated care.
The patnership reflects this model:
- Commissioners are closely involved in formulating and monitoring the framework, and review whether it remains fit for purpose, adjusting it if necessary.
- Individuals at the end of their life, together with their social network, have access to information and supportive professionals through the public health programme and the service development programme.
- Organisational and clinical processes are becoming streamlined through collaborative commissioning and service provision via integrated pathways.
- Health and care professionals come together in training, education and facilitation, and thereby learn from each other and innovate to jointly improve care.
The End of Life Partnership creates a value driven, strategic vision across a wide health and social care footprint that shapes, and is shaped by, end of life care at the front end. By developing new shared practices, it can fundamentally transform people’s experience and care.
Salli Jeynes is chief executive and Bie Nio Ong is chair at the End of Life Partnership



























No comments yet