With our models of NHS care widely seen as outdated and in need of major overhaul, the health service’s challenges are as complicated as Houdini’s tricks. But it is possible to successfully overcome them with a coordinated effort, Richard Taunt writes
How are you with to do lists?
We’ve all been there: we start with what we absolutely must do to stop our world falling apart (iron today’s work shirt), we know what we should do to make things better (buy some non-iron shirts) but are extremely unlikely to get to them anytime soon.

The NHS is in the same position.
Action is needed just to get through the mounting challenges of today. But at the same time if we don’t start acting to prepare for tomorrow we’re only going to wake up to an even bigger headache.
Unlike most of our own to do lists, there are serious consequences for the NHS not getting past the most immediate issues in front of it.
How on earth can the health service, and those at national level charged with stewarding the good ship NHS, navigate this trickiest of situations?
A recap of challenges
Let’s recap on the challenges. Quality of care remains hugely variable, causing avoidable death and misery.
Advances made over recent years are starting to go backwards, most visibly in accident and emergency departments but more worryingly largely hidden in mental healthcare.
“NHS funding” is becoming an oxymoron with providers having ended 2014-15 with a deficit of over £800m, and the NHS as a whole projecting that pressures from rising demand and input costs will grow by around £30bn by 2020-21.
‘Our models of NHS care are in need of major overhaul’
We are in the middle of a demographic revolution. Our models of NHS care are widely seen as outdated and in need of major overhaul.
Feeling queasy? And we haven’t touched on social care cuts, rising obesity levels or what we hope are just anomalous reversals in life expectancy.
How to successfully escape this mixture of short and long term challenges begins to resemble a complex Houdini trick. And like the famous escapist, the only place to start is with a thorough plan of how you are going to manage to do it.
How to manage?
This is where the NHS Five Year Forward View comes in, but only to an extent. The plaudits for the forward view went to its vision for the NHS; the implementation path to get there was largely absent.
How to simultaneously meet the challenges of today and transform for the future is a big question for the NHS, and the subject of our Health Foundation publication Shaping the Future: A Strategic Framework for a Successful NHS. The bad news is that there is no “silver bullet” we can import from another country or industry to solve all our woes.
‘We need a strategy crafted with exceptional care’
Instead what is needed is a strategy crafted with exceptional care made up of two aspects: a set of layered and interlinked plans, and the right policymaking approach.
None of the layers we suggest the strategy should focus on will come as a major surprise:
- active cost management;
- process improvements;
- new ways of delivering care;
- scientific discovery,
- technology, and skills; and
- population health.
The right balance
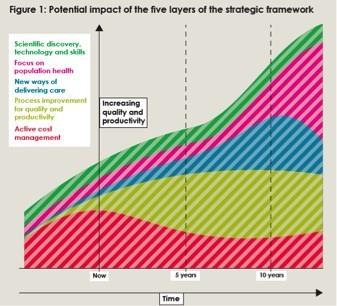
Complexity comes through the different timescale each of these elements have to deliver improvements in quality and productivity, and the size of such benefits – with the relationship between the two often being inverse (illustrated below).
For example, cost management measures (such as better procurement) have the potential to produce results within one to two years, but of a smaller magnitude to those coming from new ways of delivering care (such as the models being piloted by the vanguards) which are more likely to arrive over 5-10 years. These differences in timescale and size of impact mean that we can’t afford to ignore any of the five layers, but rather we need to strive for the right balance and for this to evolve over time.
Evidence can provide insight as to this balance, but only to a limited extent. In its place must be the right policymaking approach, one based on co-production with those who deliver clinical care and their populations, and constant evaluation of the impact of interventions.
It also requires using the full range of ways in which national policy can drive change.
‘Will the NHS deliver its to do list? It’s difficult, yes, but not impossible’
This involves careful use of the traditional policy tools which seek to “prod” organisations (such as targets and regulation), but also how both organisations and staff can be supported to improve (for example, through the rethinking of the roles of Monitor and the NHS Trust Development Authority to support trusts in making changes).
It’s clear there’s no shared view between the national bodies as to the best concoction of these different types of policy (a subject we explored in our Constructive Comfort report), but consensus is needed urgently.
Will the NHS deliver its to do list? It’s difficult, yes, but not impossible.
That the NHS has coped to the extent it has over the past five years has largely been due to the herculean efforts of NHS staff. What’s clear is that coping over the next five years and beyond won’t be possible without similar coordinated exertion from our national policymakers.
Richard Taunt is director of policy for the Health Foundation



























1 Readers' comment