To bring my trust out of of special measures we need to ensure compassion, care, transparency and learning were at the heart of every action we took
Basildon Hospital’s “good” rating from the Care Quality Commission marks the beginning of a new era. The hospital has been under intense scrutiny from the media, politicians and patients for the past five years. We can now move forward with a renewed sense of purpose and pride in the services we deliver.
‘Patient stories – good and bad – were introduced to our board meetings’
When I joined Basildon and Thurrock University Hospitals Foundation Trust in September 2012 the storm clouds were hovering. The first six months were a barrage of visits by regulators, warning notices, “risk summits” and negative media. There were concerns about our high mortality rates, poor emergency department performance, and delays in recognising and acting when patients’ conditions were deteriorating.
We needed to ensure compassion, care, openness, transparency and learning were our core principles. I am confident we are moving in the right direction and last month’s CQC inspection report was a watershed moment when we became the first of the Keogh review trusts to be taken out of special measures.
Here is what worked for us to get to this point.
Being visible, listening and acting
We increased our visibility on the wards and listened to the views of patients and their carers. Patient stories – good and bad – were introduced to our board meetings and we met more regularly with complainants. We also started monthly listening surgeries for patients and relatives.
Communication channels were opened up to establish regular forums for discussion with staff. We now have a meeting in the hospital restaurant every morning, led by an executive director, where all staff are invited to raise patient safety concerns and receive support from colleagues to address them.
- Basildon removed from special measures
- HSJ celebrates inspirational women in healthcare
- See who is on the HSJ Inspirational Women 2014 list
- Download a free PDF of the top 50 list
- Join the debate using hashtag #HSJWomen
Our patient advice and liaison service was moved to the front door of the hospital, led by a newly appointed senior nurse.
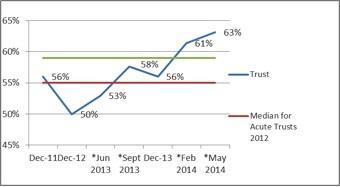
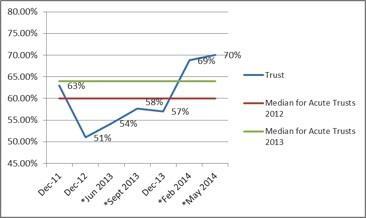
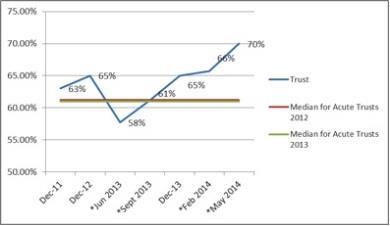
We started a quarterly mini staff survey, which shows a rapidly improving performance, particularly in the friends and family test (see graphs below).
I would recommend this organisation as a place to work
If a friend or relative needed treatment I would be happy with the standard of care provided by this organisation
When errors, near misses or incidents are reported, my organisation takes action to ensure that they do not happen again
Putting clinicians at the heart of decision making
Our senior team was restructured to ensure it had strong representation from clinicians. We wanted to ensure doctors and nurses were at the heart of decision making. This ensured patient safety and experience were at the top of our agenda and that no decisions were made which could adversely impact on the quality of care.
We are now investing in this multiprofessional group with a development programme run by Professor Richard Bohmer from Harvard Business School.
Good governance
We emphasised the need for people to understand their responsibilities and how to escalate concerns. This enabled us to learn from serious incidents and have good systems in place for sharing experiences “from the board to the ward”.
We stripped out unnecessary meetings to ensure we focused on the stuff that really matters. Our incident reporting has moved from being among the lowest in the country to among the highest. More than 150 clinicians have been trained in route cause analysis to ensure the quality of our investigations and this will continue.
Getting our workforce right
We employed 200 more clinical staff and placed a huge emphasis on delivering the best care 24/7, with consultants’ rotas ensuring senior cover out of hours. We were able to do this by converting some of our expensive nursing agency staff into permanent roles.
As one of the first trusts to act on the recommendations of the Francis report, the majority of appointments were made from within the UK. This will prove to be a challenge as other trusts follow suit.
Making sure patient safety is the priority
It’s obvious – but we needed to remind ourselves why we’re here. Our mortality rates had been outlying for several years and we needed to better understand the drivers for this.
‘We built confidence inside and outside the organisation by doing what we said we would do and being open’
We focused on the emergency care pathways and introduced proper handover processes to manage continuity and risk.
We worked with colleagues in UCL Partners to identify early signs of deterioration among patients in hospital and interventions such as the national early warning score chart and treatment escalation planning have led to a significant reduction in cardiac arrests.
We also invested in senior staff out of hours. Our in-house IT team developed a system to help us track mortality in real time that accurately predicts the summary hospital level mortality indicator, giving confidence that the many and varied actions were having an impact.
These steps have resulted in reduced crude mortality and our actual SHMI is now within the expected range.
Focus on emergency care
Our inability to cope with the rising demand through our emergency department was debilitating and we spent most of winter 2012-13 on “black alert”. Non-urgent elective work was delayed between January and March 2013.
We took the decision to invest in additional beds on site and build a new modular ward in six months. We focused on pathways and introduced new frailty and primary care front end models. A strong performance in the second half of 2013-14 resulted in the hospital achieving the 95 per cent target for the year and this has been sustained.
Communicate
We built confidence inside and outside the organisation by doing what we said we would do, by being open and honest and making use of the expertise of others.
Our local newspaper is a daily and was becoming increasingly critical of us without properly understanding the issues. It was important to actively engage with them and the rest of the media. We introduced monthly planned briefing sessions and took opportunities to be open through local TV and radio interviews, put a human face to the stories and explain our commitment to change.
This approach was also important with Monitor and the CQC, as well as clinical commissioning groups and local stakeholders. Regular communication and delivering on, or ahead of, deadline built confidence and trust. This was reflected in the shift we experienced – from being challenged to being supported.
Clare Panniker is chief executive of Basildon and Thurrock University Hospitals Foundation Trusts



























10 Readers' comments