Payment by results in the NHS has had success, but it is time to encourage local freedom to create a new blend of payment methods, says John Appleby
“New outcomes-based payment models replace bureaucratic targets with simple outcomes that reward the long term success that the public wants to see, while giving people on the front line more freedom to get the job done.”
No, this is not a quote from the Department of Health circa 2003, but from the Home Office this year. Its new payment scheme, called payment by results, concerns a number of Home Office offender, drug and alcohol recovery programmes.
‘Payment by Results looks like a system whose time has come. And it started in the NHS’
Elsewhere in Whitehall, the Department for Communities and Local Government has used Payment by Results to fund its “troubled families” scheme, and the Department for International Development has launched a similar initiative as a way of financing overseas aid.
Payment by results looks like a system whose time has come. And it started in the NHS.
Not without success
In many ways, payment by results in the NHS has been a tremendous success. The scale of its implementation has been impressive, rivalling most other countries’ attempts to implement similar systems. The technical issues that had to be addressed, from defining the “product” to designing the fixed tariff without inducing too much instability across the NHS, were substantial.
Payment by results now accounts for 40-50 per cent of an average trust’s total income − in total nearly £30bn of NHS spending − and includes upwards of 1,300 separate types of work.
A national evaluation of the system showed it has succeeded in boosting activity, reducing length of stay and encouraging more day case over inpatient work. It appears not to have reduced quality of care.
And yet the more we have got to know about how payment by results and similar payment methods in other countries have operated - coupled with big changes in the economic, financial and policy context in which the NHS operates since the system was originally designed - the more there seems a case for a rethink.
‘Payment systems cannot do everything. They are one of many levers that can be used to achieve change’
A key goal for payment by results in those days when the NHS was receiving one of the biggest funding boosts in its history was to encourage hospitals to do more work to reduce waiting times.
But now and for the foreseeable future, the goals − and certainly the financial environment − have changed. A payment system that rewards doing more for more is less and less appropriate.
Different approaches
There are some general lessons we have learned too. First, payment systems cannot do everything. They are one of many levers and policy tools that can be used to achieve change.
Second, one size does not fit all. Different services will need different ways of paying providers in order to meet different sets of objectives. Related to this is a third point that any payment system needs to be flexible, to deal with unexpected shocks or unpredicted outcomes.
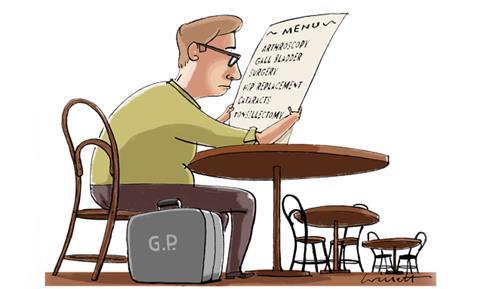
There needs to be flexibility too between national rules and frameworks and local discretion and experimentation. A knee replacement operation for the otherwise healthy 50-year-old and ongoing episodic care for a 75-year-old with multiple long-term needs require different payment approaches to give the right incentives to providers to deliver high quality, cost effective care.
‘Payment by results now looks bitty, fragmented and increasingly complex’
Finally, we need to find out more about how different payment systems operate in practice in different situations. Further developments in payment approaches will need to be supported by high quality data and analysis.
Any system not underpinned by reliable data and analysis will lack compliance, or risks leading to unintended and unwanted side effects.
More local freedom
The NHS Commissioning Board and the system regulator Monitor will soon be taking on the design and pricing functions of payment by results. So how should they approach this job?
Things could carry on more or less as they have over the last few years, with incremental development of the payment system alongside some approaches better suited to current needs, such as bundled and year of care payments.
However, as the King’s Fund argues in our new report, Payment by Results: how can payment systems help to deliver better care?, it would be better to encourage local experimentation within a national framework.
Commissioners and providers would be required to seek approval for, and commit to evaluate the impact of, local variations. The board and Monitor would provide technical support and track the innovations adopted.
The lessons from abroad, and to an extent in the NHS, are that no payment system fits all circumstances and that it can be very hard for the centre to keep up with necessary developments and changes. Payment now looks bitty, fragmented and increasingly complex.
Not just allowing, but actively encouraging and supporting, more local freedom to innovate new payment methods would be a way to generate the sort of “blend” of payment systems that the NHS now needs.
John Appleby is chief economist at the King’s Fund



























3 Readers' comments