Improved procurement is seen as an important means of generating a good proportion of the cost efficiencies the health service needs to find. Ingrid Torjesen reports
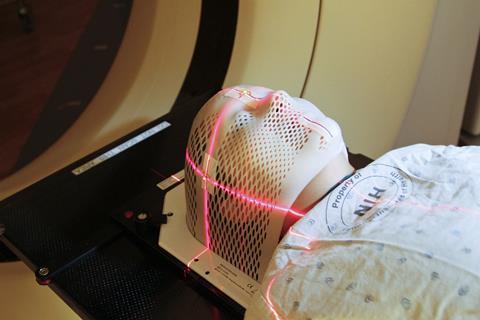
CT scan
Every year the NHS spends more than £22bn on goods and services - roughly 30 per cent of its operating costs.
With the NHS expected to find £1.5bn a year in efficiencies, smarter procurement is seen as a means for generating a good proportion of these savings.
“We are tackling financial waste and inefficiency in the NHS and believe smarter procurement could save £1.5bn,” says health minister Dan Poulter.
“We are already making progress - NHS Supply Chain will save £150m by next year, our new league tables are helping trusts save hundreds of thousands of pounds on everyday items and we have plans to help them make even more savings, ensuring value for taxpayers’ money.”
‘Smarter procurement could save the NHS £1.5bn’
Last July Dr Poulter launched the NHS Procurement Atlas of Variation website to help trusts see the differences in the amounts they spend on everyday items such as gloves, disinfectant wipes and stationery.
The website reveals clear room for improvement on procurement but to make it a reality will involve a number of groups. This includes regional NHS bodies, key opinion leaders, politicians, procurement channels, professional healthcare bodies, manufacturers and trade associations.
It also includes trusts themselves. Take, for instance, capital equipment. For the past two years, the Department of Health has offered a loan of £300m for the purchase of this. But even with that and other such initiatives, trusts will still have to find about half of the overall cost, says Mark Hitchman, chair of the Association of Healthcare Technology Providers for Imaging, Radiotherapy and Care.
He explains: “Much of the imaging equipment used also comes with the high cost of building alteration, air conditioning requirements, and so forth, which can be half the cost of the asset and typically cannot be borrowed.”
More from the Redefining innovation series
Meeting requirements
What of the role for suppliers in supporting better procurement? Giles Maskell, president of the Royal College of Radiologists, says that it is important that any third party supplier engages with trusts and the clinicians using the equipment to ensure that what is purchased meets their requirements.
Dr Maskell would also like an independent unit commissioned to evaluate different pieces of equipment. “At the moment individual trusts spend a lot of time and effort evaluating different models of scanner,” he says.
‘A system that allows mid life upgrades and optional add-ons would be more cost effective’
“If there were a system for carrying out some of the evaluation independently across the NHS, rather than every trust doing it for themselves, that would make an awful lot of sense and would save a lot of time and effort.”
Another potential area for change is in the contracts under which capital equipment is bought. As the financial positions of trusts have got more difficult under austerity measures, replacement of such equipment has suffered.
rocurement is an opportunity to address this, Dr Maskell says. “There is no doubt that we are seeing the installed base of CT and MRI scanners getting older year by year,” he explains. Older machines are more prone to breaking down and potentially deliver higher doses of radiation to patients.
Karl Blight on making NHS procurement smarter
This series of articles has focused on “redefining innovation”. We have been exploring ways that the NHS can innovate to meet the evolving challenges of modern healthcare.
Previous articles in the series have looked at topics including the appropriate integration of care across the NHS and how to tackle the impact of its ageing installed base of medical equipment.

In this final piece, we continue on the medical equipment front - investigating the NHS’s procurement climate, and asking whether there are smarter, more effective, more innovative ways to ensure the current system is attuned to improving patient outcomes.
With the NHS needing to find £1.5bn in procurement savings by 2016 - as set out in, Better Procurement, Better Value, Better Care, the procurement development programme for the NHS - we have the opportunity to look at how the system should evolve to help meet that challenge.
Like the NHS, GE is a large organisation with a long history. In any enterprise like this, there are times when established processes need fine tuning or redesigning to better meet the demands and requirements of the economic and global environment, and to better align with the changing needs of customers.
Our experience is that identifying the need for change is part one. Part two, effective implementation, can be more challenging but is essential in a rapidly changing world.
For the NHS, so many parties are impacted by the procurement process - from technology and service providers such as GE Healthcare to radiographers or end users of a system, to a chief operating officer or head of department concerned about the flow and throughput of patients, right through to cost conscious procurement managers.
Does everyone in the process share the same goal? Are their targets aligned in the right way? Are time, efficiency savings and long term benefits being considered or only short term costs? Could improvements be made that would ultimately benefit the broader system or, more importantly, the patient?
Are representatives with similar goals from different hospitals communicating with one another about their needs and experiences? It seems as though many agree there is a need for change. We hope this article will be a catalyst for further discussion that enables the NHS to improve outcomes for patients.
Karl Blight is general manager for northern Europe at GE Healthcare.
Proofing for the future
Most scanners procured for the NHS have very high specifications because they will have to last for a very long time and perform a huge variety of complex tests. Trusts face enormous difficulties in obtaining funding for upgrades once a piece of equipment has been purchased, so they try to “future proof” from the outset, and some of the options will never be used.
Mr Hitchman explains: “A system that allows mid life upgrades and optional add-ons [for example: adding cardiac capability to a CT scanner at three-years-old only when the clinical demands are there] would be more cost effective.”
Meg Hillier, Labour MP for Hackney South and Shoreditch and a member of the Commons public accounts committee, which provides an oversight of government procurement, agrees. She argues planned upgrades should be written into contracts from the outset. She also emphasises the importance of not giving all the business to one supplier, even if they are the cheapest.
“You can then actually lose competition in the market and the cost savings aren’t necessarily there longer term,” she says.
‘To unlock the greatest savings it is important to determine the most efficient patient pathway’
Procurement involves more than just striking a good deal at the outset, Ms Hillier emphasises. “The whole approach to procurement needs to be looked at differently” because it is also about logistics - making sure that trusts have the items they need when they need them - and procuring efficiently, she says.
It is important to really look at how the supply chain works so as to determine what is best procured centrally, what is best procured locally, and what is best where the deal is struck centrally but the day to day to purchase is undertaken locally, she says.
To unlock the greatest savings it is also important to determine the most efficient patient pathway.
Achieving these savings long term may require some investment up front, Mr Hitchman points out. For example, using cardiac CT to triage patients with acute chest pain in accident and emergency can quickly identify those with acute coronary syndrome and those with non-cardiac causes, reducing hospital stays and avoiding other expensive tests.
The DH should pilot studies to generate evidence of such potential savings, he suggests.
“Some companies, if asked, might even underwrite the project, should the hypothesis of savings from innovation not be met.”


























No comments yet