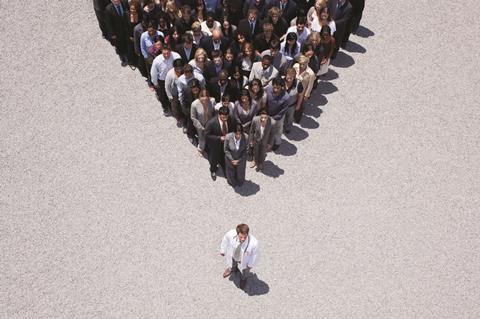
If place is going to become the way the NHS is run, the involvement of clinicians as leaders needs to become essential, write Ted Adams and Rich Taunt
Let’s start with some universally acknowledged truths.
One: areas, or places, make a better starting point for planning healthcare than organisations. Two: if you don’t have clinicians leading your changes, the odds of anything actually happening become rather slim. Three: just creating new posts and labelling them as “place-based clinical leaders” isn’t going to help very much. This is complex business, and requires a mindset shift from all clinical leaders, not just those with “STP” or “ICS” in their job title.
But then the truth runs out. It would be quite handy if we knew exactly how to nurture and develop this new form of clinical leadership (and quickly), but we don’t. We’re into new territory, without a blueprint, and where no single area can claim to have a fully articulated strategy as to how they’re planning to do this. Given that a number of studies, by the King’s Fund and others, have shown the challenges in achieving clinical engagement in sustainability and transformation partnerships, we probably shouldn’t be too surprised that clinical leadership has been even harder still.
So we’re going to have to build as we go, drawing learning from system leadership and the creative efforts of a number of areas which are leading the way. The good news is that it’s likely all of the necessary pieces already exist; the tricky bit is working out which way they go together. It’s possible to draw out three themes.
1. Don’t expect a job description. Working as a clinical leader across a patch will require dealing with problems (and potential solutions) which are ambiguous, unclear and above all complex. Clinicians are taught both to be highly expert, and to understand where this expertise begins and ends. By and large, once you know where all of the organs are, you don’t expect them to move. Not quite the case with NHS management structures, let alone the informal politics which swim around them. If clinical leadership involves more complexity than clinical work, then place-based clinical leadership raises the bar yet again. Knowing how to navigate such waters is job number one.
2. Find some new shoes. Being any sort of place-based clinical leader will bring you into contact with a far broader mix of people than organisational leadership. Suddenly you’re interacting with people who may have no idea what your specialty even means. To be successful, you’re going to need to find ways to understand what makes very different people tick (and what ticks them off). One way is to copy the GP-Consultant exchange model developed in the south east, pairing clinicians across the primary, secondary care divide. Running since 2015, the exchange has been credited in building far greater empathy between colleagues and helping resolve longstanding tensions. Another way is the Melting Pot Lunches we run at Kaleidoscope, bringing diverse groups together from across health and care to discuss key topics (all over a supermarket meal deal).
3. Learn together. Let’s get real – the amount of time place-based clinical leaders are going to have to devote their new responsibilities is unlikely to be enough. Finding efficient ways to gain new skills, broker new relationships, and find new insights is key. This is likely to be why so many of the areas leading the way have looked to ways to get people to learn together. This could be a one-off session on a particular topic, a development programme, or longer. For example, the 2020 Leadership Programme developed in Frimley has provided professional development in a multiprofessional setting, with learning from the army, Microsoft and beyond. The Darzi Fellowship in London, and Kent, Surrey and Sussex, has sought to do likewise over a whole year.
None of this is rocket science. But it does require some priority, resource and time. These resources are fiercely contested, not least by pressures to improve performance, and limit deficits. Given this, it’s easy to understand how place-based clinical leadership slowly slips to becoming a nice-to-have rather than a necessity. Understandable perhaps, but unhelpful. If place is going to become the way the NHS is run, the involvement of clinicians as leaders, not bemused bystanders, needs to become essential.





























No comments yet