Despite the NHS staff surveys revealing a range of issues that need to be tackled, staff typically say that nothing happens to fix them. A shift of consciousness amongst leaders is needed to help build the belief that things can be different. By Hannah Forbes
Thousands of NHS staff, asked at events over the last couple of years, say without hesitation that 60-70 per cent of their personal energy at work is lost as a result of bureaucracy, broken processes, poor management, and things that get in their way.
Stop and think about that for a minute… and after a grimace and a sigh, imagine the potential if we could get that back.
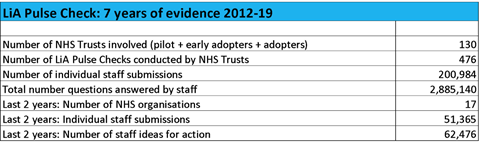
This shocking revelation is backed up by more than 200,000 NHS staff responses to the Listening into Action Pulse Check, which measures how engaged and empowered staff feel. Over the past seven years, without exception, the lowest scoring question in every trust is: “Day-to-day frustrations are quickly identified and resolved.”
In other words, those things they say sap their energy at work. “Feeling valued” and “Processes that support me” are right down there too.
In the past two years alone, staff across acute, mental health, community and specialist trusts have shared more than 60,000 ideas for action they say would make a difference to them, their ability to do their jobs, and the experience of their patients and service users.
Themes and ideas are consistent, regardless of the type of trust.
When you get traction on basic needs, such as management of day-to-day frustrations, fixing broken processes, and communication, everything changes
The saddest and most exciting realisation here – depending on which way you look at it – is that these are easy, do-able ideas to go at and there is an endless supply of low hanging fruit.
So far, so good. Most trusts can say that they have listened to staff – through the National Staff Survey, listening events, local surveys, etc – but it’s what happens next that matters. Unfortunately, staff typically say that nothing happens next, that the same issues are raised time and time again with no response, that there is never any action.
No wonder levels of frustration are so high, no wonder staff are weary, no wonder morale is low. Forget about the big national issues like staffing numbers and money, even the simple things – those within our gift to change – are not being addressed.
How is this okay? Not only for staff who often feel they are working with their hands tied behind their backs, but because this directly and indirectly impacts trust performance in terms of quality and safety of patient care, and operational efficiencies such as retention and staff sickness.
So what can we do about it?
What you achieve depends on what you put in
The solution involves a shift of consciousness amongst leaders, and the building of belief that things can be different amongst staff.
This doesn’t require a year of planning, it’s a bungee jump decision based on the recognition that a real, sustained improvement to staff engagement will impact culture and make everything else possible.
Once you get it, there’s no going back and life is forever different. Then it’s just about doing it well.
Here’s a recent example to show what is possible… Chesterfield Royal’s 3rd LiA Pulse Check results show they are up once again (all questions, every year) on all 15 questions, including: 62 per cent up on baseline on “removing day-to-day frustrations”, 39 per cent up on “feeling valued”, and 43 per cent up on “able to influence change”.
They received 2,500 ideas and comments this year from staff about simple actions to make things work better; have made hundreds of changes, many led on the ground by teams themselves; achieved the second highest response rate in the last National Staff Survey at 71.9 per cent; shifted from “bottom left” to “top right” on the National LiA Scatter Map within two years, up 101 places on the associated NSS League Table; and have been shortlisted for the HSJ Award for Staff Engagement this year.
The culture change is palpable. This is what is possible and the kind of results that many trusts are starting to see.
Seven success factors for any NHS trust
So, what are the top insights and success factors…
-
Not “another initiative”
This is about a fundamental shift, not a trendy project for the year that will tick a few boxes. A scattergun approach will not work.
You need a framework and a route map for: engaging staff, harnessing their ideas, building belief that you mean it, bringing all leaders, managers and corporate services on board to enable and unblock the way for staff; powering up clinical and support teams with uncomplicated ways to make the changes to their services that they want to see; and engaging staff trust-wide on exciting “hot topics” they say matter, like: improving patient safety, cutting bureaucracy and paperwork, outpatients of the future, winter pressures, and use of space, communication that works for us.
And have your best ever communication campaign to shout about it all from the rooftops so that the changes are palpable and to “fuel” the spread.
-
Learn from Maslow and build a solid foundation
When you get traction on basic needs, such as management of day-to-day frustrations, fixing broken processes, and communication, everything changes. Evidence from around 100 trusts shows that when these scores go up, so do those relating to patient care, feeling valued, ability to influence change, and feeling connected.
Think Maslow’s hierarchy of needs – you can’t self-actualise if your basic needs are through the floor!
-
Break what isn’t working and start what will
Want to get back some of that 60-70 per cent energy at work that staff say is lost to them? There are literally thousands of simple changes that staff say will make a difference for them, and the enthusiasm you will generate by taking this seriously is priceless…
-
“We have to jump through hoops to fill a post”: remove or drastically simplify vacancy control processes and trust staff (who save lives!) to get on with it
-
“We need a business case/permission to buy small items we have a budget for”: give teams a purchase card and let them get on with it (and watch the buying psychology in your trust improve overnight)
-
“It takes ages to find a parking space when we need to pick up test results”: provide 30-minute parking spaces for community staff pick up and drop off
-
“There is no access to drinking water where we work”: Hello?? This (among many other things) is a basic human need. Just fix it!
-
An enabler for quality improvement
Quality improvement is everywhere and the intent is honourable. But if you have a culture in which staff do not feel engaged and empowered, they will be reluctant to get involved and you will see limited results.
Back to Maslow’s hierarchy: you need a positive climate in which they believe things are changing, can see evidence of that, appreciate that leaders are listening, and are able to crack on with their own actions.
Once you have traction, more complicated changes that require more technical improvement methodologies have a better chance of success and, vitally, can be owned by the teams themselves instead of feeling done to them.
-
The only purpose of a survey is to measure impact
It’s what you do in between that counts. NHS staff are sick and tired of responding to surveys and seeing nothing change, only to be asked the same questions again three or six or 12 months later. “The definition of insanity is doing the same thing over and over again and expecting different results”, as the saying goes.
The National Staff Survey is a given. The one other trust-wide survey done each year should be used to engage on local, staff-led action – stop everything else.
Make the action – by teams, trust leadership, and corporate services – visible to all, to build belief and create “pull”.
-
If it’s not clinically led you may as well not bother
This is healthcare and everything everyone does is – or should be – about delivering the best care to patients and service users. There is – or should be – no other agenda.
Bringing a whole workforce on board to change an organisation is not easy, but you will go nowhere without them. Unfortunately, they have seen many initiatives come and go, and had their hopes dashed far too many times.
This has to be different every step of the way, and it must be led by the doctors, nurses, AHPs and other healthcare professionals who sit at the heart of everything we do, and everything the NHS is about. Show them that the key sponsors navigating this journey are their people.
It can’t be an “HR thing”. Put the full weight of the trust behind it with 100 per cent unwavering commitment and leadership from the executive team. Now we have something to work with.
-
Measure it
This is not soft stuff, it’s what delivers the hard stuff. Get wind in your sails by unblocking the way and impressing staff.
Use this as the basis to attract teams who would love to impact waiting times or safety or integrated services or whatever matters to them and their patients. Measure and story-tell the ‘before and after’ far and wide.
Shine a light on the porter who got a mirror put up in a corridor to make it easier to transport patient trolleys, or the healthcare assistant who got an unused area transformed into a staff break – and watch others follow.
Show off the managers who inspire and support their teams to lead change. Track staff sickness, retention, agency spend, National Staff Survey movement, and how engaged staff are feeling.
When the outcomes are clear and the results beyond dispute, those who are cynical will start to believe, those who weren’t interested will prick up their ears.
Last month, the new CEO at South London and Maudsley Foundation Trust, David Bradley, started on a journey like this, with these success factors in mind. He announced on his arrival that staff engagement is his top priority, launching their journey at the monthly senior leaders’ meeting.
They expected 30 people, 100 turned up: many frontline staff, trade union reps, black and minority ethnic, executives and the improvement team. This trust has many challenges but, no kidding, some people were actually dancing as they came into the room.
They had heard about it and wanted to be part of it. Gate crashers welcome!
Engaging and empowering staff is a long-term campaign, not a project. It is part of the organisational DNA, not an initiative
It was buzzy, positive and – best of all – full of hope. Within the next four weeks, they achieved a 61 per cent response rate to their LiA Pulse Check – the highest response ever to anything.
Other CEOs have embedded and sustained these approaches for longer periods of time and to great effect. A case in point is Dame Jackie Daniel who, over the past 8-10 years, has developed her “FlourishAtWork” approach, tailoring and applying it to organisations she has led.
This includes University Hospitals of Morecambe Bay FT – where LiA was the starting point – and The Newcastle upon Tyne Hospitals FT.
For both an organisation dealing with some specific challenges and an organisation rated outstanding by the Care Quality Commission, Jackie has been clear that staff feeling valued and empowered at work underpins all aspects of the trust’s performance, from patient care to leading innovation and change.
One aspect of “Flourish” has been to shape the employee wellbeing agenda by adopting a holistic approach to creating a healthy workplace. This focuses on the key themes of a well workforce, being valued and recognised, and behaviour and culture.
Importantly, in Newcastle, “FlourishAtNewcastleHospitals” sits at the heart of the trust’s operating framework and strategy, and will be a key element of strategic development in every part of the organisation for the next five years and beyond. It is a top priority.
Engaging and empowering staff is a long-term campaign, not a project. It is part of the organisational DNA, not an initiative.
It’s a movement, not fad. Take a bungee jump.
Hannah Forbes, staff engagement expert, founder and CEO of Listening into Action (LiA) with thanks to Dame Jackie Daniel, CEO at Newcastle-upon-Tyne Hospitals FT, David Bradley, CEO at SLaM, and Simon Morritt, CEO at Chesterfield Royal Hospital Trust until August 2019.































1 Readers' comment